Herpesviruses II
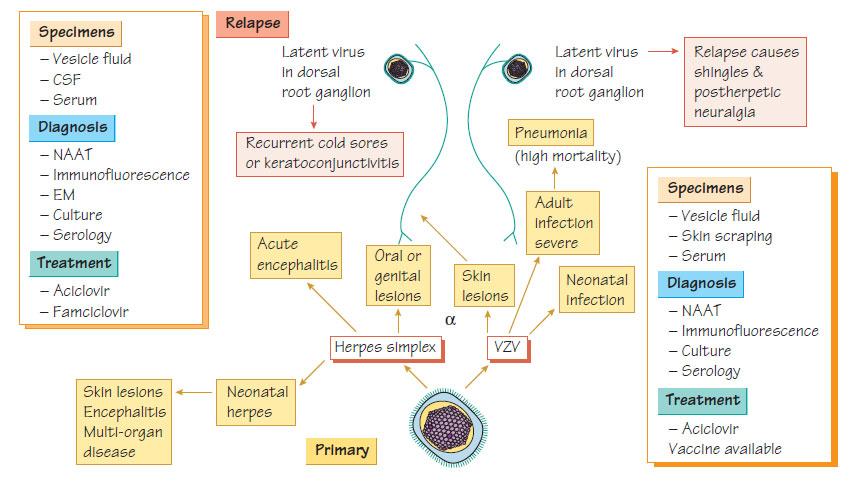
Herpes simplexPathogenesis and Epidemiology
- Transmitted by direct contact.
- Invades skin locally producing skin vesicles by its cytolytic activity.
- Remains latent in the sensory ganglia.
- Reactivation is triggered by physical factors (e.g. infection, sunlight), or psychological stress.
- Cell-mediated immunity controls infection, therefore immunocompromised patients are at risk of reactivation and severe infection.
- Herpes simplex virus 1 (HSV-1) is often asymptomatic, but young children commonly develop fever, vesicular gingivostomatitis and lymphadenopathy.
- Adults with infection may exhibit pharyngitis and tonsillitis.
- Primary eye infection produces severe keratoconjunctivitis; recurrent infection may result in corneal scarring.
- Primary skin infection (herpetic whitlow) usually occurs in traumatized skin (e.g. on fingers).
- Severe encephalitis may occur (see Infections of the central nervous system).
- Mother-to-child transmission perinatally may result in a generalized neonatal infection including encephalitis.
- HSV-2 infection causes painful genital ulceration that lasts up to 3 weeks and is associated with recurrence.
- Genital herpes is an important cofactor in the transmission of HIV.
- Meningitis is an uncommon complication of primary type 2 infection.
A nucleic acid amplification test (NAAT) of vesicle fluid, genital or mouth swabs is the standard diagnostic method, although the virus grows readily and can be visualized by electron microscopy (EM). The ratio between serum and CSF antibody may indicate local production and can help in the diagnosis of HSV encephalitis. MRI or CT scans of the brain may detect temporal lobe lesions that are typical of herpes encephalitis.
Treatment
Topical, oral and intravenous preparations of aciclovir and other agents with better oral absorption, including valaciclovir and famciclovir, are available. Encephalitis is treated with intravenous aciclovir.
Varicella zoster virus
Varicella zoster virus (VZV), which has only one serological type, causes the acute primary infection known as chickenpox and its recurrence, which is called shingles.
- VZV is found in the vesicle and transmission is by contact and airborne spread from patients with vesicles.
- The attack rate in non-immune individuals is very high (>90%).
- The incubation period is 14-21 days.
- Infection is commonest in children aged 4-10 years.
- Recovery provides lifelong immunity.
- The virus remains latent in the posterior root ganglion and in 20% of patients will reactivate with lesions in the related dermatome, causing shingles.
- Shingles lesions contain VZV and are infectious to non-immune individuals who are at risk of developing chickenpox.
- It is impossible to contract shingles directly from chickenpox or other cases of shingles.
- The discomfort of chickenpox comes from the rash.
- Systemic symptoms are mild.
- Lesions, which appear in crops usually 2 or 3 days apart, affect all parts of the body, including the oropharynx and genitourinary tract, and progress through macules and papules to vesicular eruptions which, following rupture, develop a crust and spontaneously heal.
- The rash lasts for 7-10 days, but complete resolution may take as long again.
- Haemorrhagic skin lesions that can be life-threatening may occur.
- Secondary infection with Staphylococcus aureus or Streptococcus pyogenes may also require treatment.
- VZV pneumonia is more common in adults, especially in immunocompromised individuals, and has a high mortality; survivors may recover completely or may have respiratory impairment.
- Postinfectious encephalitis, which is usually minor, can occur, but there is also a rare fatal form.
- Maternal transmission through contact with vaginal lesions during birth can result in severe neonatal infection.
- Shingles is a painful condition that usually affects older people or immunocompromised individuals.
- Ocular damage may follow the involvement of the ophthalmic division of the trigeminal nerve.
- Up to 10% of shingles episodes will be followed by Postherpetic neuralgia, a very painful condition that may last for many years and can be associated with suicide.
- Both chickenpox and shingles are usually diagnosed clinically.
- Laboratory diagnosis is by NAAT.
- Staining of fluid from a vesicle may show characteristic giant cells.
- VZV may be visualized by EM or cultured.
- Serology is important to determine the immune status of patients and staff in outbreaks.
Treatment and Prevention
- Aciclovir or valaciclovir may be used for both adult chickenpox and shingles.
- Postherpetic neuralgia may be reduced by early treatment.
- Pain may be severe and require referral to a pain clinic.
- A live attenuated-virus vaccine is available and recommended for non-immune healthcare workers.
- Zoster immune globulin (ZIG) is given to those in close contact with infection who are at risk of serious disease (e.g. neonates, pregnant women and immunocompromised individuals).