HIV infection and AIDS
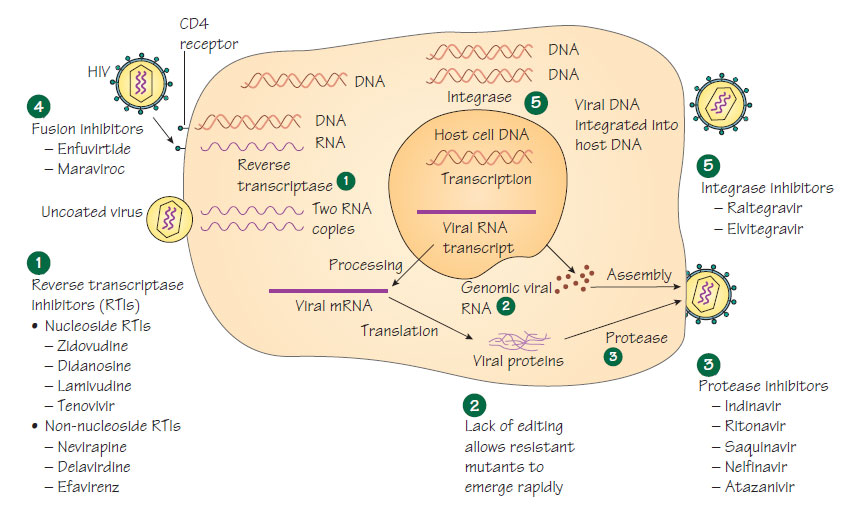
Human immunodeficiency virusHIV is a spherical, enveloped RNA virus. It is a retrovirus, using reverse transcriptase to produce a DNA copy from viral RNA that is incorporated into the host nucleus to become the template for further viral RNA. Three genes are required for viral replication: gag, pol and env. HIV is classified as a lentivirus. There are two types that are pathogenic for humans: HIV-1, which is most common; and HIV-2, which is found mainly in West Africa and appears to be less virulent.
Infection with HIV has spread worldwide, transmitted by the parenteral and sexual routes. Infection is most common in individuals at high risk of sexually transmitted diseases, especially those where genital ulceration is common. In developed countries, the main risk groups are intravenous drug users and men who have sex with men; heterosexual transmission is less common but does occur. In developing countries, HIV spreads mainly by heterosexual transmission and through unscreened transfusions or use of contaminated medical equipment. Infection can be transmitted from mother to fetus.
Pathogenesis
The virus principally infects cells with a CD4 receptor (e.g. T cells and macrophages). Viral replication results in progressive T-cell depletion and diminished cell-mediated immunity. Different virus strains display varying affinities for cells that express particular chemokine receptors. Lacking T-cell help, B-cell function is also reduced. HIV causes damage to neural cells and stimulates cytokine release that may also cause neurological damage. Many of the clinical signs of AIDS are caused by secondary infections, which occur when the CD4 count falls.
A few weeks after infection, a mononucleosis-like syndrome may develop with rash, fever and lymphadenopathy. There is a primary viraemia after which the viral load reduces to a steady state, the concentration ('set-point') being related to outcome. The CD4 count declines and, if untreated, reaches a point (<0.2 � 109/L) where CD4 function is sufficiently compromised for secondary infections and malignancies to develop, a condition known as acquired immune deficiency syndrome (AIDS). Use of highly active antiretroviral therapy (HAART) delays this development. Bacteria Mycobacterium tuberculosis, Mycobacterium avium- intracellulare (see Pathogenic mycobacteria), Salmonella, Streptococcus pneumoniae.
Protozoa Toxoplasma gondii, Cryptosporidium parvum, Isospora belli, microsporidia.
Fungi Candida spp., Cryptococcus neoformans, Pneumocystis carinii.
Viruses Varicella zoster virus (VZV), human papovavirus.
Malignancy Kaposi sarcoma (HHV-8), non-Hodgkin's lymphoma.
Children with HIV infection are especially vulnerable to childhood viral infections (e.g. measles) and recurrent bacterial infections (e.g. pneumonia).
Diagnosis is by detection of HIV-specific antibody using two different immunoassay methods. As seroconversion may take up to 3 months, an initial negative result should be repeated. HIV viral load and CD4 count are tested on presentation and regularly during care. Resistance should be tested initially and if a change of therapy is necessary. HLA B5701 and tropism are tested if treatment with abacavir or CCR5 antagonist is contemplated.
Treatment
Antiretroviral drugs are described in Virus structure, classification and antiviral therapy . Therapy aims to maintain the virus at fewer than 50 copies, prevent the emergence of resistance, restore immunological function and prevent transmission. Treatment is initiated for any patient with opportunistic infection or when the CD4 count is <0.350 � 109/L, although patients with higher counts may benefit. It is also recommended for pregnant women who do not meet these criteria (see Congenital and perinatal infections). Patients must be aware of the lifelong commitment. Because RNA viruses lack efficient mechanisms for genetic proof-reading, mutations arise rapidly and patients develop drug resistance quickly. Regimens must be adapted to an individual patient's medical and social condition. Patients infected with resistant virus require tailored regimens. Regimens may include an NNRTI and two NRTI, or a combination that includes a protease or integrase inhibitor. As the immune system starts to recover with treatment, known as immune reconstitution, symptoms from opportunistic infection can worsen due to the effects of the enhanced immune reaction.
- Avoidance of partners who have a high-risk factor and unprotected intercourse (e.g. by using barrier contraception).
- Screening of blood products.
- Health education and free needle-exchange programmes for intravenous drug users.
- Antigenic diversity has frustrated vaccine development.
- Antiretroviral prophylaxis should be given for infected needlestick injuries.
- Transmission from mother to child can occur (see Congenital and perinatal infections).