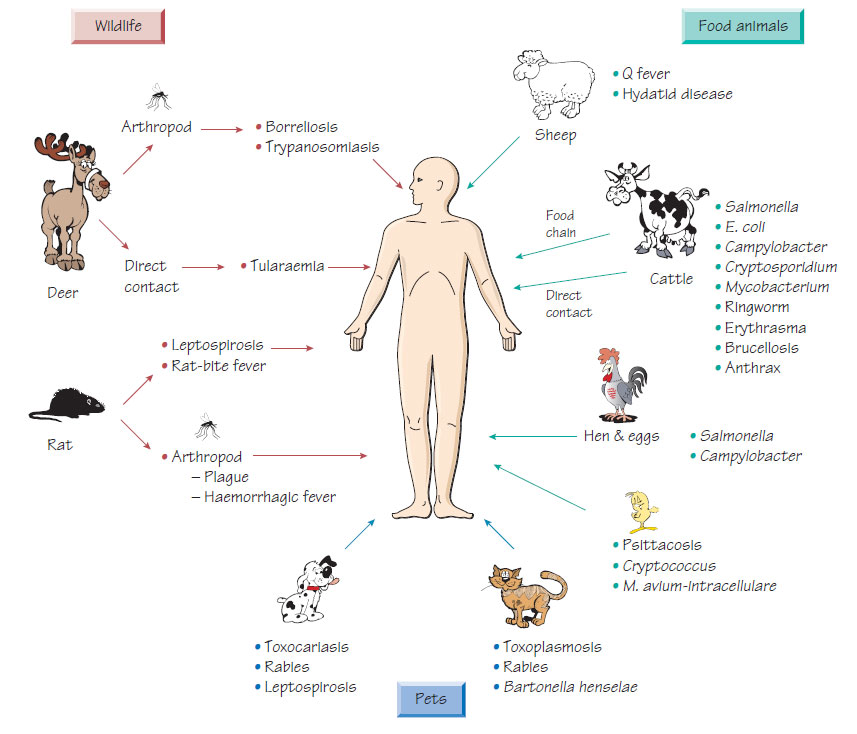
Zoonoses
A zoonosis is an infection acquired from an animal source.- Infection can occur when humans enter the animal environment (e.g. when camping).
- Transmission can be via vectors such as mosquitoes (e.g. Japanese B encephalitis).
- Farming and pets are an important source of zoonotic infection.
Viral zoonoses
More than 100 animal viruses can cause human disease (e.g. Herpes simiae, a monkey pathogen, which causes severe encephalitis, or avian 'flu, both of which are associated with high mortality). Other viral zoonoses are discussed in Tropical, exotic or arbovirus infections.
Rat-bite fever
Rat-bite fever is caused by either Streptobacillus moniliformis or Spirillum minus inoculated by the bite of a rat.
- The incubation period is 3 days to 3 weeks.
- Inflammation occurs at the site of the bite, with associated lymphangitis and regional lymphadenopathy.
- Generalized maculopapular rash, fever, headache and malaise may occur.
- Polyarthritis occurs in 70% of cases.
- Endocarditis is the most serious complication.
- Diagnosis based on bacterial isolation or nucleic acid amplification test (NAAT).
- Treatment is usually with penicillin.
Anthrax
See Listeria, Bacillus, Corynebacterium and environmental mycobacteria .
Caused by Yersinia pestis, infection is endemic in rodents in remote rural areas. Rarely, epidemics may develop that spread worldwide (e.g. the 'Black Death'). The organism is transmitted both between rats and to humans by the rat flea, Xenopsylla cheopis. The incubation period is short; the disease has an abrupt onset characterized by fevers and toxaemia. The regional lymph glands draining the site of the bite become greatly enlarged (buboes) and septicaemia is accompanied by generalized haemorrhage. Pneumonic plague is a rapidly fatal pneumonitis that can be transmitted by the respiratory route.
Plague is diagnosed clinically in areas where it is endemic. Direct smear of a lymph gland aspirate, blood culture and NAAT are used for diagnosis. Treatment is with tetracycline, chloramphenicol, aminoglycosides or ciprofloxacin. The mortality rate of pneumonic plague is high. There are concerns that it may be used as a bioterrorism weapon.
Borreliosis is transmitted from rodents or deer by ticks particularly in open forest habitat (e.g. the New Forest) or by lice (see Spiral bacteria).
Toxoplasmosis
The cat is the definitive host of Toxoplasma gondii but the organism infects a wide range of animals, including sheep, cattle and humans. Infection is acquired by ingestion of oocysts from infected cat faeces or from tissue cysts in infected meat (e.g. undercooked beef).
Dermatophytes
Dermatophytes that are natural pathogens of animals can spread to the human population by direct contact (see Filamentous fungi).
Toxocariasis
Toxocara canis is an ascarid parasite of dogs. The parasite eggs are excreted in the faeces of infected dogs and mature in the soil. Human ingestion occurs when food is contaminated by the soil or when personal hygiene is poor (e.g. poor hand washing). The larval stages hatch in the intestine, invade the host and migrate to the liver and lungs. They are unable to develop into adults but migrate throughout the body causing fever, hepatosplenomegaly, lymphadenopathy and wheeze. If the larva migrates into the eye, sight may be permanently damaged by the local inflammatory response of the retina. The diagnosis is made serologically using a specific enzyme immunoassay (EIA). The disease is usually selflimiting but, if symptoms are severe, treatment with albendazole may be beneficial. Ocular lesions should first be treated with steroids to diminish the inflammatory response; the role of antihelminthic treatment is less certain.
- Caused by infection with Bartonella henselae.
- There is a 10-day incubation period following a cat scratch or bite.
- A papular lesion may develop at the site.
- Regional lymphadenopathy occurs.
- Symptoms resolve slowly over a period of 2 months, but a more chronic course may ensue.
- Disseminated infection occurs more commonly in immunocompromised individuals.
- The diagnosis is usually made clinically but it can be confirmed serologically by immunofluorescence or EIA. Culture requires a prolonged incubation period; NAATs may also be used for diagnosis.
- Treatment with azithromycin, tetracyclines or rifampicin may be beneficial.
Two species of parasite are responsible for human hydatid disease: Echinococcus granulosus and Echinococcus multilocularis. Dogs are the definitive host of E. granulosus, harbouring the tapeworm stage. The eggs, which are passed in the faeces, are ingested by the intermediate hosts (e.g. sheep or rodents) and multiple cysts develop in the liver and lungs. The cycle is completed when dogs eat infected tissues. Humans are accidental hosts. The disease is common in sheep-farming areas. Echinococcus multilocularis is found in foxes, wolves and dogs; rodents act as the intermediate hosts.
Pathogenesis and Clinical features
Cysts act as space-occupying lesions in the liver, lungs, abdominal cavity or central nervous system. The cysts of E. multilocularis lack a definite cyst wall and spread in the tissue.
Diagnosis
Cysts may be demonstrated by ultrasound or CT. EIA for both antibody and antigen is available.
If possible, hydatid cysts should be surgically removed. Albendazole is given to kill the germinal layer of the cyst and praziquantel to reduce the viability of protoscolices. Puncture, aspiration, injection of chemicals and re-aspiration (PAIR) is seen as an alternative to surgical excision. Cyst rupture can lead to multiple cysts in the abdomen, or to anaphylaxis