Yeast infections
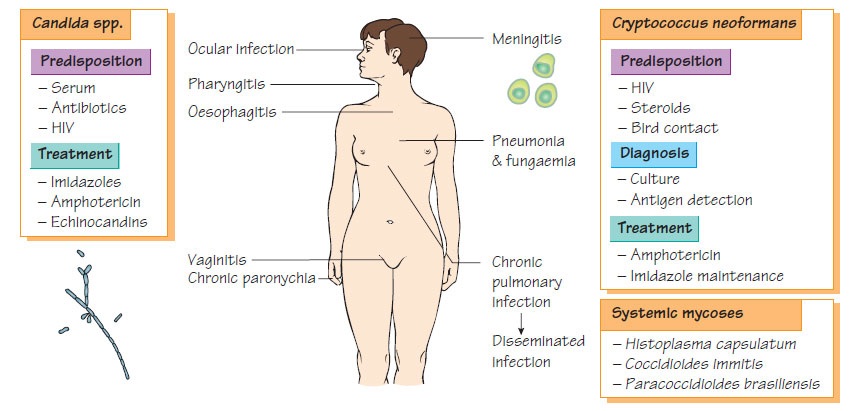
Fungi cause a wide range of diseases, ranging from cutaneous dermatophyte infections to invasive infection in the severely immunocompromised patient. They may have a yeast-like morphology (see below), or be filamentous (see Filamentous fungi).Candida spp.
Candida spp. are widely distributed in the environment. They form part of the normal commensal population of the skin, gastrointestinal tract and female genital tract. Following the use of broadspectrum antibacterial agents, fungal overgrowth may develop into infection. Patients with immunodeficiencies are particularly susceptible to this progression. Most infections are caused by Candida albicans. Infection with other species such as C. tropicalis, C. parapsilosis, C. glabrata and C. pseudotropicalis are a problem in immunocompromised patients because they may be resistant to the antifungal agents used in therapy or prophylaxis.
Although these organisms possess melanin, adhesins and extracellular lipases and proteinases, they have only modest capacity to invade. Infection occurs when the natural resistance provided by the normal bacterial flora is altered by antibiotics, or where there is a severe loss of immune function.
Clinical features
Candida spp. cause pain and itching with creamy curd-like plaques on mucosal surfaces that bleed when removed. Skin and nail-bed infections are common. In immunocompromised patients, pharyngitis and oesophagitis can be severe; the associated dysphagia may lead to weight loss and is an AIDS-defining illness. Systemic invasion is common in neutropenic patients. Candida spp. may also cause systemic and line-associated infection following broadspectrum antimicrobial therapy in intensive care patients.
Diagnosis is by microscopy, culture or nucleic acid amplification test (NAAT). The significance of each isolate is determined in relation to the overall clinical picture. Species identification is by biochemical testing or increasingly by sequencing the 18S rRNA gene.
Antifungal susceptibility
Candida spp. are susceptible to amphotericin, with the exception of C. lusitaniae. They are usually susceptible to the imidazoles (e.g. fluconazole) and to 5-flucytosine.
Cryptococcus neoformans
Cryptococcus neoformans is a saprophyte and animal commensal; the composition of pigeon faeces favours its growth. It is a rare cause of chronic lymphocytic meningitis in patients with lymphoma, those taking steroid or cytotoxic therapy and those with intense exposure, such as pigeon fanciers. Cryptococcus is an important pathogen in patients with T-cell deficiency.
The pathogenicity depends on an antiphagocytic capsule, melanin production and several lytic enzymes.
Clinical features
Infection usually presents as subacute meningitis, although pneumonia and fungaemic shock are recognized. In patients with AIDS, relapses are common and lifelong suppressive therapy is necessary.
Laboratory Diagnosis
Infection is diagnosed by microscopy in CSF using Gram stain or India ink, or by detection of the capsular polysaccharide antigen by latex-agglutination. It can be cultured and identified by biochemical tests or 18S rRNA sequencing.
Treatment
Liposomal amphotericin is the treatment of choice and flucytosine and fluconazole may also be used.
Pityriasis versicolor
Malassezia furfur infects the stratum corneum, causing brown, scaly macules. Patients with AIDS may develop severe dermatitis. Topical application of antifungal agents is usually successful.
Five main species of yeast are associated with systemic infection: Histoplasma capsulatum, H. capsulatum var. duboisii, Blastomyces dermatitidis, Coccidioides immitis and Paracoccidioides brasiliensis. These organisms have a defined geographical distribution: south-west USA, South America and Africa. Infection is acquired by the respiratory route. Severe disease is more likely in patients with reduced cell-mediated immunity.
Clinical features
Although usually asymptomatic or self-limiting, pulmonary or cutaneous infection may disseminate in infants or immunocompromised patients, causing severe illness.
Laboratory Diagnosis
These infections are diagnosed by microscopy and culture of blood, sputum, CSF, urine or pus. The organisms are hazardous and should be handled in a specialized containment facility.
Treatment
Patients with severe disease may be treated with amphotericin B.
Azoles
The azole group of compounds (clotrimazole, miconazole, fluconazole and itraconazole) act by blocking the action of cytochrome P450 and sterol 14α-demethylase. This latter enzyme allows the incorporation of 14-methyl sterols into the fungal membrane, instead of ergosterol. Resistance can develop during long-term treatment. Clotrimazole and miconazole are frequently used as topical preparations for minor infections.
Fluconazole
Fluconazole can be given orally, topically and parenterally. It is widely distributed, crosses the blood-brain barrier and is active against Candida and Cryptococcus but not against filamentous fungi. It is used for the prophylaxis and treatment of cryptococcal infections and treatment of superficial and systemic candidiasis. Although well tolerated, it may cause liver enzyme abnormalities and has significant drug interactions, increasing the serum concentration of phenytoin, ciclosporin and oral hypoglycaemic agents and reducing the rate of warfarin metabolism.
In addition to being effective against Candida spp., C. neoformans and Histoplasma, itraconazole also displays activity against filamentous fungi, including Aspergillus and the dermatophytes. It is indicated in the treatment of invasive candidiasis, cryptococcosis, aspergillosis, superficial mycoses and pityriasis versicolor. Resistance is rare. It is well absorbed and can be given orally, achieving high tissue concentrations.
Voriconazole and posoconazole
Voriconazole is a broad-spectrum triazole that is active against many yeasts and moulds including Aspergillus. It has been reported to have a better success rate in proven invasive Aspergillus infection than amphotericin, but treatment is associated with transient visual disturbance. Posoconazole has a wide spectrum of activity. Further agents are in development.
This synthetic fluorinated pyrimidine inhibits Candida spp., C. neoformans and some moulds. The drug disrupts protein synthesis. It is well absorbed orally and can be given intravenously. Adverse events include bone marrow suppression, thrombocytopenia and abnormal liver function tests. Resistance develops rapidly with monotherapy.