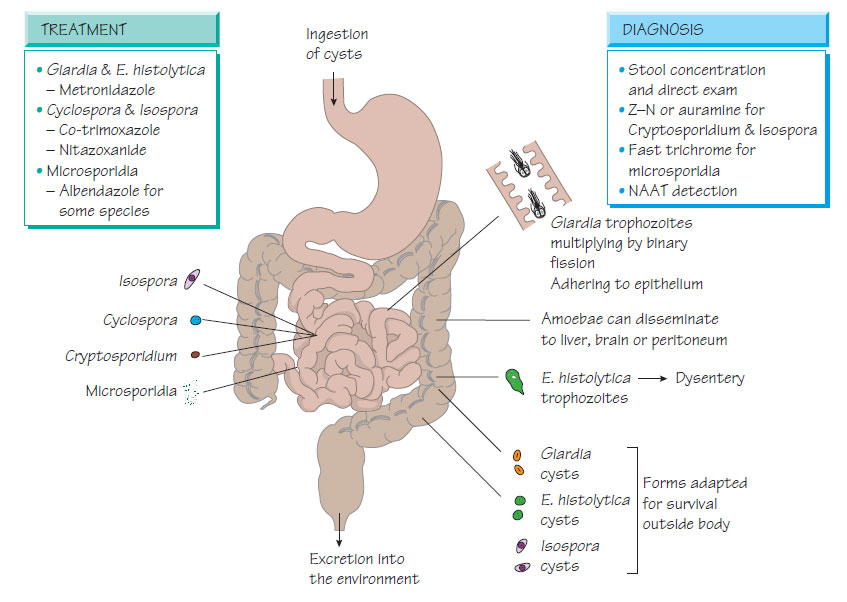
Intestinal protozoa
Entamoeba histolyticaEntamoeba histolytica infects the large intestine and is found mainly in developing countries. It is transmitted by the faecal-oral route. The organism causes disease through production of cysteine protease and amoebapore, an epithelial cytotoxin. It is morphologically identical to E. dispar, which does not cause disease.
Clinical features
The onset is insidious with little systemic upset: the patient is ambulant but passes frequent small-volume, offensive, bloody stools. Abscesses may develop in the liver or, more rarely, abdomen, lung or brain.
- Rectal ulceration is seen on sigmoidoscopy.
- Trophozoites are demonstrated in ulcer biopsies.
- Three stool specimens for microscopy, antigen detection and nucleic acid amplification test (NAAT).
- CT and ultrasound for abscesses.
- Serology - may detect liver abscess, but not intestinal infection.
Treatment
- Metronidazole for intestinal infection and abscess.
- Diloxanide furoate or paromomycin kills the chronic cyst stage.
Prevention and control
Steps to ensure that water is boiled and food adequately cooked will reduce the risk of amoebic infection.
Giardia lamblia infection occurs worldwide where poor sanitation allows water supplies or food to be contaminated with cysts from human or animal faeces.
Pathogenesis
Trophozoites multiply in the jejunum and attach to the intestinal wall by a sucking disk. The mechanism for Giardia diarrhoea is uncertain and may relate to induced apoptosis. Giardial cysts are excreted in the faeces and survive well in the environment.
Clinical features
These may include:
- bulky, offensive, fatty stools;
- anorexia, crampy abdominal pain, borborygmi and flatus;
- weight loss;
- lactose intolerance or fat malabsorption;
- recurrent attacks of infection in patients with IgA deficiency.
- Three concentrated stool samples for microscopy.
- Aspirated jejunal contents can be examined for motile trophozoites.
- Enzyme immunoassay (EIA) and NAAT methods are more sensitive than microscopy.
Treatment
Metronidazole or tinidazole are used. New therapeutic options include albendazole and nitazoxanide. Secondary malabsorption and vitamin deficiency may require investigation and treatment.
Cyclospora cayetanensis
Infection occurs in subtropical and tropical regions from contaminated water supplies; outbreaks from imported soft fruit and fresh herbs have been reported.
Cyclospora are found inside vacuoles within the epithelium of the jejunum. There is inflammation, villous atrophy and crypt hyperplasia leading to malabsorption of vitamin B12, folate, fat and D-xylose.
Clinical features
- Infection takes the form of watery diarrhoea.
- A 'flu-like illness and weight loss may also occur.
- Infection is self-limiting, but may last for weeks with continuing fatigue, anorexia and weight loss.
- A prolonged, severe, relapsing disease occurs in individuals who have AIDS.
Diagnosis and Treatment
- Microscopy for oocysts in stools.
- NAAT methods are available.
- Co-trimoxazole is an effective treatment, with nitazoxanide as an alternative.
Cryptosporidium parvum is a zoonotic coccidian parasite that is transmitted by milk, water and direct contact with farm animals. It is naturally resistant to chemical disinfectants, surviving water purification. Person-to-person spread can occur with intimate contact. Infection is common in children and individuals with AIDS. It may interfere with the glucose-stimulated sodium pump in the small intestine, leading to fluid secretion.
Clinical features
- Infection usually produces self-limiting, watery diarrhoea with abdominal cramps.
- Profuse, prolonged diarrhoea in immunocompromised individuals may cause life-threatening fluid and electrolyte imbalance.
- Biliary tree, gallbladder and respiratory tract involvement may occur.
- Demonstration of cysts by microscopy.
- Antigen detection or NAAT.
- Nitazoxanide may improve clearance of pathogens but Management should aim to reverse immunodeficiency (e.g. treatment of AIDS).
Isospora belli
Closely related to Cryptosporidium, Isospora belli presents with a similar clinical picture, usually following tropical travel. Diagnosis is by microscopy of stool. Treatment is with co-trimoxazole; fluoroquinolones or nitazoxanide.
Microsporidia
These are small intracellular protozoa that infect insects, plants and animals. Enterocytozoon bieneusi, Encephalitozoon cuniculi, Encephalitozoon hellem, Septata intestinalis, Pleistophora and Nosema have been implicated in human infection, usually in immunocompromised patients.
Enterocytozoon bieneusi and S. intestinalis infect epithelial cells of the small bowel and are associated with diarrhoea. E. cuniculi infects macrophages, epithelial cells and vascular endothelial cells in the brain and the kidney plus renal tubular cells. It is associated with hepatitis, peritonitis, diarrhoea, seizures and disseminated infection. Before the advent of HIV infection, microsporidia infection was very rare.
Diagnosis and Treatment
Microscopy using fast trichrome, calcofluor white and Ziehl- Neelsen stains can be used. Sensitive NAATs are available to demonstrate organisms.