Tissue helminths
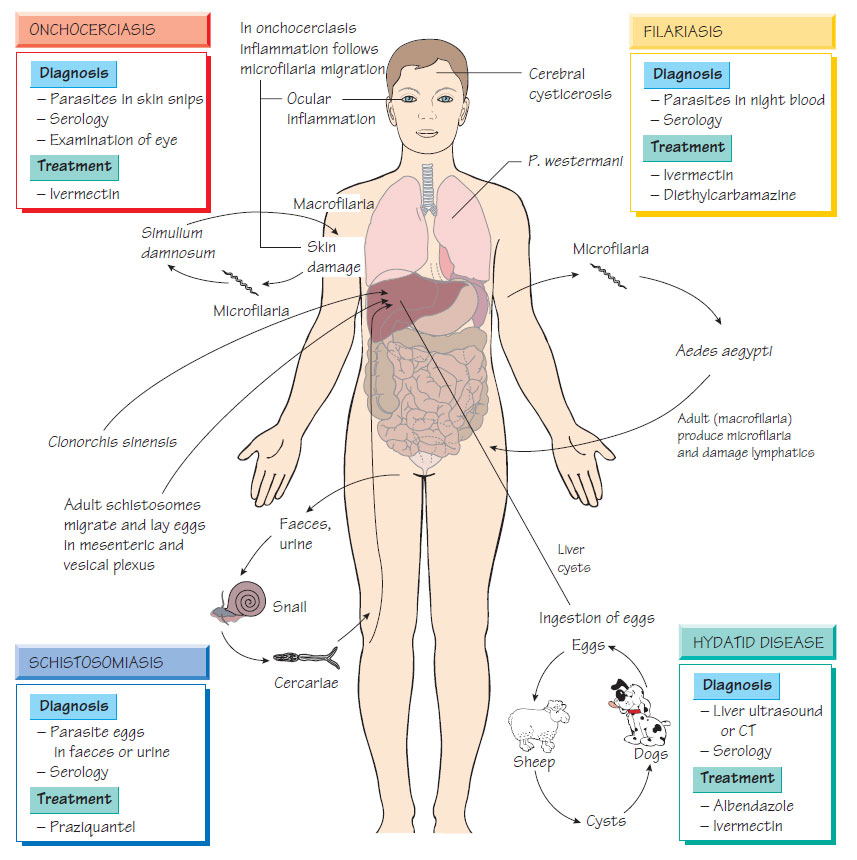
SchistosomiasisThree species infect humans: Schistosoma mansoni (Africa and South America); S. japonicum (Far East); and S. haematobium (Africa). Eggs are excreted in the faeces and urine of infected humans. In areas with poor sanitation, the eggs hatch, releasing a miracidium that invades a snail. After development in the snail, the schistosome cercariae emerge into the environment. They actively penetrate intact skin and develop into male and female adult worms that migrate to the superior, inferior mesenteric or vesical plexus, depending on species, where they lay eggs.
- Initial infection: fever, hepatosplenomegaly, rash and arthralgia.
- Egg expulsion: bloody diarrhoea or haematuria.
- Later: symptoms and signs are caused by the fibrotic reaction to the eggs in the liver (hepatic fibrosis and portal hypertension), the lungs (pulmonary fibrosis) and bladder. Space-occupying lesions in the brain and spinal cord may lead to seizures.
Diagnosis
Microscopy for eggs in stool, urine, rectal snips or other tissue biopsy. An enzyme immunoassay (EIA) that detects antischistosomal antibody is useful, especially in travellers, and antigen detection methods are available as research tests.
- Avoidance of contaminated water and the wearing of appropriate clothing when working in the fields.
- Control programmes that target snails.
- Mass treatment can control the disease if sufficient resources are available.
Filariasis
Lymphatic filariasis is caused by Brugia malayi and Wuchereria bancrofti and transmitted by the mosquito Aedes aegypti throughout the tropics. Onchocerciasis is caused by Onchocerca volvulus and transmitted by the blackfly, Simulium damnosum, in West Africa and South and Central America. Loa (loiasis) is caused by Loa loa and transmitted by Chrysops flies in West Africa.
Lymphatic filariasis is characterized by acute attacks of fever and lymphoedema, which may be complicated by secondary bacterial infection. After repeated attacks lymphatic vessels are permanently damaged, leading to lymphoedema in the leg, arm or scrotum. Inflammation arises from the response to endobacteria (Wolbachia spp., related to Rickettsia) that infect the filariae. Onchocerca adults are located in nodules and microfilariae migrate in the skin, resulting in pruritus and dry, thickened skin. Inflammation in the eye causes blindness. Loiasis is less damaging and diagnosis is based on fleeting subcutaneous swellings, known as Calabar swellings. Infection may be associated with fever and abnormalities of renal function.
- Lymphatic filariasis: identification of microfilariae in a peripheral blood sample taken at midnight.
- Onchocerciasis: microscopic examination of 'pinch biopsies' taken from any affected area, plus the shoulder-blade, buttocks and thighs. If the biopsy is negative, a 50-mg dose of diethylcarbamazine will induce increased itch (the Mazzotti reaction).
- Loiasis: Loa loa is detected in daytime blood films.
- EIA is also used for diagnosis.
Treatment
Treatment of filarial infection may stimulate an acute inflammatory reaction.
- Lymphatic filariasis: diethylcarbamazine or ivermectin together with albendazole.
- Onchocerciasis: ivermectin (the addition of tetracycline enhances the effect on microfilarial load by sterilizing the adult worms).
An international onchocerciasis control programme is under way, using mass treatment of whole populations with ivermectin and doxycycline. Lymphatic filariasis is prevented by mosquito-control measures.
Hydatid disease
See Zoonoses .
Clonorchis sinensis (Opisthorchis sinensis)
Infection is acquired, mainly in the Far East, by eating undercooked fish that contains metacercariae. The adults live in the bile ducts, and eggs are passed in the faeces. Light infections are usually asymptomatic, but heavier infections result in cholangitis and pancreatitis; biliary obstruction and cirrhosis may develop. Cholangiocarcinoma is a late complication. The diagnosis is made by identifying the characteristic eggs in faeces. Patients may be treated with praziquantel. Infection is prevented by adequate cooking of potentially infected fish.
Humans are accidental hosts of this sheep and cattle parasite. The infective stage is found on freshwater plants such as watercress which, if eaten without cooking, can result in infection. The larvae hatch in the intestine; after maturation and migration, the adults are located in the liver. Patients present with fever and right upper quadrant pain. Low-grade biliary symptoms and liver fibrosis may denote continuing infection. Treatment is with praziquantel.
Paragonimus spp.
Paragonimus spp. infect different organs: P. westermani, lungs; and P. mexicanus, brain. This rare infection follows the ingestion of undercooked crustaceans. Acute, non-specific symptoms, such as fever, abdominal pain and urticaria, are followed by specific symptoms and signs, such as chest pain, dyspnoea and haemoptysis or central nervous system signs. Diagnosis is made by identification of the characteristic eggs in sputum, imaging, serology or tissue biopsy. Lung fluke is treated with praziquantel; cerebral disease with a combined surgical and medical approach.