Congenital and perinatal infections
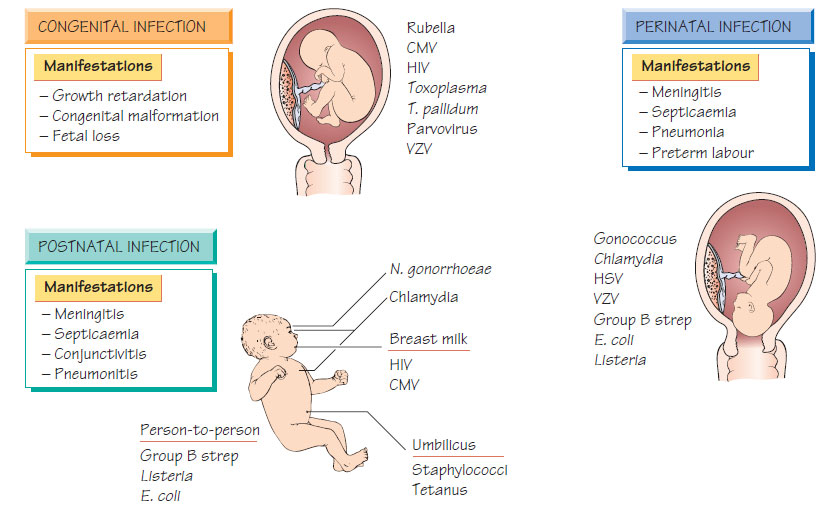
Infection may be acquired across the placenta (intrauterine infection) or contracted during the process of birth or by direct contact with maternal body fluids. Prolonged rupture of the membranes predisposes to fetal infection. Infection can also be transmitted to the neonate after birth from the mother or other contacts.Congenital rubella
Jaundice associated with hepatitis is often the first sign of congenital rubella. Haemolysis and thrombocytopenic purpura are also common, as is a low-grade meningoencephalitis. Some babies have evidence of metaphyseal dysplasia. Infected infants have low birthweight and fail to attain their expected developmental milestones. There is a high mortality in severely affected infants. Patent ductus arteriosus, cataracts, deafness and retinal pigment dysplasia may be present. Rubella IgM is positive and persists until the third month of life. The risk to the fetus from maternal infection during the first trimester is more than 60% and some parents will opt for termination of pregnancy. Later the risk is much lower (2% after 20 weeks) and the balance between the chance of fetal damage and the desirability of termination should be considered carefully.
Infection occurs in less than 1% of births, of which 1% are severely affected. The risk of infection is highest during the first trimester. It presents with prematurity, low birthweight, hepatomegaly, splenomegaly, thrombocytopenia, prolonged jaundice, cerebral irritability, fits and/or abnormal muscle tone or movement. Microcephaly and sensorineural deafness are the most common problems. Other problems include cerebral calcification, hemiplegia, psychomotor retardation, chorioretinitis and myopathy. Diagnosis depends on demonstrating IgM antibodies or cytomegalovirus (CMV) excretion during the first 20 days of life.
Congenital and intrapartum herpes simplex infections
Primary herpes simplex infections may be accompanied by viraemia when transplacental infection can occur. Infants born with congenital infection tend to have severe disease, with pneumonitis, meningoencephalitis, hepatosplenomegaly and cytopenias. Only a few will demonstrate herpetic skin or mucosal lesions. Treatment with aciclovir reduces mortality from 80-90% to 10-15% and should not wait for laboratory confirmation. Primary infection may be contracted at birth from maternal genital herpes. Skin, conjunctival, oral or genital lesions develop within a few days, with dissemination in 50% of cases. Treatment is with intravenous aciclovir.
Varicella embryopathy follows maternal infection during the first or second trimester of pregnancy; it is transmitted in less than 3% of infected pregnancies. Cicatricial contracture of a limb with hypoplasia, microcephaly or microphthalmia may occur. Nonimmune women exposed to chickenpox should be offered postexposure prophylaxis with zoster immune globulin (ZIG) within 10 days of exposure. Neonatal varicella occurs when the mother develops chickenpox within 1 week of delivery. As neonatal mortality is up to 40%, the neonate should be given ZIG within 48 h of birth if possible and treated with aciclovir if infection develops. Normal immunoglobulin given to the mother will not protect the infant. A vaccine is entering clinical use in some countries.
Transplacental transmission of Listeria monocytogenes occurs during a maternal infection that is often not apparent. Infection in early pregnancy often results in fetal death; later infection is associated with premature labour. Severe bacteraemia, associated with hepatosplenomegaly, meningoencephalitis, thrombocytopenia and pneumonitis, usually complicates neonatal infection. Intrapartum exposure may lead to neonatal infection during the first 2 weeks of life, usually with meningitis and bacteraemia. Blood, CSF, placental tissue and lochia should be cultured. Infected mothers and infants may be a source of infections in the postnatal ward and should be isolated. Ampicillin with or without the addition of gentamicin (for 2-6 weeks) is the treatment of choice.
Syphilis
Congenital infection is now rare as a result of antenatal screening. Affected babies are feverish with features similar to secondary syphilis: rash, condylomata and mucosal fissures. Osteochondritis may cause pain. Persistent rhinitis ('snuffles') is common. Diagnosis is confirmed by dark-ground microscopy of mucosal or skin lesions. Specific IgM or antibodies persisting after 6 months indicate infection. Late manifestations appear between 12 and 20 years: deafness, optic atrophy or paretic neurosyphilis. Other features include bossing of the frontal bones, chronic tibial periostitis, notching of the incisors, 'mulberry' deformity of the first permanent molar and a high arched palate. The treatment of choice is benzylpenicillin.
The incidence of toxoplasmosis varies internationally; it is uncommon in the UK, but common in France. Transplacental infection occurs in a third of affected pregnancies. Infection in the first and second trimester is more likely to cause significant fetal disease: the fetus may be stillborn, die soon after birth, or have cerebral calcification, cerebral palsy or epilepsy. Chorioretinitis may not be evident until after birth and may be the only feature. Maternal toxoplasmosis is confirmed by specific IgM antibodies or by seroconversion. IgM antibodies may also be demonstrated in affected neonates. Treatment with spiramycin may reduce the risk of transplacental infection but does not affect the outcome of fetal disease.