HDL and “Reverse Cholesterol Transport”
Epidemiological studies show a strong inverse relationship between HDL levels (HDL cholesterol or apo-A1) and risk of CHD. Even a small increase in HDL is significantly correlated with a reduction in the risk of premature heart disease.Unlike VLDL and chylomicrons, HDL is formed from its protein and lipid components in the bloodstream and interstitial fluids. The major apolipoproteins of HDL are apo-A1 and apo-A2. These proteins are secreted from hepatocytes and intestinal epithelial cells independently and also as minor components of VLDL and chylomicrons. Apo-A1 and apo-A2 bind to phospholipids. Phospholipids are available from the surface of VLDL after lipolysis. In addition, cells are able to efflux phospholipids through the action of ABCA1.
ABCA1 is a membrane transport protein belonging to a large family of ATP-binding cassette proteins. These proteins include the cystic fibrosis transmembrane receptor, the sulfonylurea receptor (a pancreatic β-cell protein involved in insulin secretion), and the multidrug resistance transporter proteins. It is thought that ABCA1 mediates the efflux of phospholipid and/or cholesterol from cells, thus making them available for association with apolipoproteins to form HDL. Its crucial role in this process was established by the discovery that two types of severe inherited HDL deficiency syndromes are caused by mutations in ABCA1 (see Fig. 12).
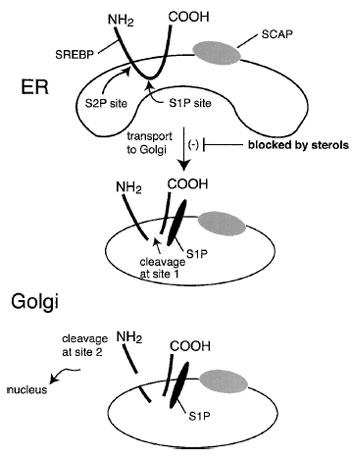 |
| Figure 12 The reverse cholesterol transport hypothesis. Extraheptatic cells accumulate cholesterol through the uptake of LDL and modified forms of LDL through the LDL receptor, other members of the LDL receptor family, and/or scavenger receptors. These cells efflux cholesterol and phospholipids to the extracellular milieu through a process facilitated by a membrane transporter, ABC1. Free apo-A1 interacts with the phospholipid and cholesterol to form HDL3 particles. LCAT esterifies the cholesterol to form discoidal HDL2 particles which then interact with the SR-B1 receptor at the surface of hepatocytes. Through that interaction, cholesterol esters are selectively taken up into the hepatocytes and hydrolyzed. The free cholesterol is then secreted into the bile or converted to bile acids. Much of this cholesterol is then excreted in the feces. |




