Antibacterial therapy
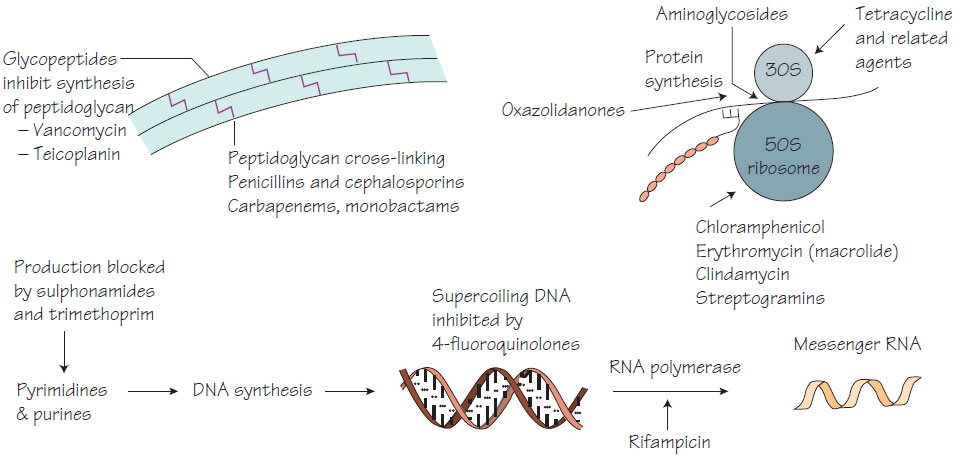
Principles of antibiotic therapyAntibiotics aim to kill organisms while causing no harm to the patient - this concept is known as selective toxicity. It is best achieved by inhibiting bacterial functions that are not present in human cells, for example the peptidoglycan of bacterial cells is inhibited by penicillin. The difference between the dose necessary for treatment and that which causes harm is usually large and is known as the therapeutic index. The aminoglycosides are exceptions to this because doses just above the therapeutic level can be toxic. While all antimicrobials have potential unwanted effects, fortunately serious unwanted effects are not frequent.
Antibiotic choice depends on the:
- infection site: sufficient concentrations of antimicrobial may be difficult to achieve in some sites such as abscesses, bone, the CSF or areas with poor blood supply and some sites with low pH inhibit certain antibiotics (e.g. aminoglycosides);
- organism: identification of the organism predicts the natural history of the infection, thereby allowing treatment optimization;
- susceptibility pattern: Streptococcus pyogenes is invariably susceptible to penicillin, but other organisms such as Acinetobacter and Pseudomonas are resistant, so antibiotics should be chosen to cover the resistance pattern of all the potential pathogens;
- severity of infection: severe infections require antibiotics to be given by the parenteral route;
- history of allergy: a previous allergic response may limit the choice of antibiotic;
- likelihood of unwanted effects: for example, aminoglycosides should be used with care in patients with pre-existing renal disease.
Antibiotics are usually taken orally in mild infections, but intravenous therapy is usually required in severe infections, such as septicaemia, to ensure adequate antibiotic concentrations are achieved. Intravenous therapy may also be chosen for patients unable to tolerate oral therapy. Topical administration is suitable for skin infections. More rarely, antibiotics are given per rectum (e.g. metronidazole for surgical prophylaxis) or intravaginally as pessaries. Children require palatable liquid formulations to maximize adherence.
Monitoring therapy
It is possible to measure the concentration of an antibiotic in the serum or at the site of infection (e.g. in the CSF for meningitis). This may be necessary to:
- ensure that there are adequate therapeutic concentrations at the site of infection;
- reduce the risk of toxicity, which is important where the therapeutic index is low (serum levels of aminoglycosides should be measured in serum taken just before and 1 h after intravenous or intramuscular dosage, which allows the dose to be adjusted according to normograms and careful adherence to guidelines, e.g. for a high peak the dosage may be reduced or for a high trough level the medication is given less frequently);
- assist in the management of an infection with intermediate susceptibility (if inhibition of an organism occurs only at high antibiotic concentrations, it is important to ensure sufficient concentrations are found at the site of infection, e.g. in Pseudomonas meningitis, antibiotic concentrations should be measured in the CSF);
- study the pharmacokinetics of the drug (treatment plans are based on knowing the absorption, distribution and protein binding of drugs). In the development of new antibiotics the way in which the new agent is absorbed and distributed throughout the body is studied by careful sampling.
Mild gastrointestinal upset is probably the most frequent side effect of antibiotic therapy. Rarely, severe allergic reactions may lead to acute anaphylactic shock or serum sickness syndromes.
Gastrointestinal tract
Antibiotic activity can upset the balance of the normal flora within the gut (β-lactams are especially likely to do this) resulting in overgrowth of commensal organisms such as Candida spp. Alternatively, antibiotic therapy may provoke diarrhoea or, more seriously, pseudomembranous colitis (see Clostridium).
Skin
Cutaneous manifestations range from mild urticaria or maculopapular, erythematous eruptions to erythema multiforme and the life-threatening Stevens-Johnson syndrome. Most cutaneous reactions are mild and resolve after discontinuation of therapy.
Haemopoietic system
Patients receiving chloramphenicol or antifolate antibiotics may exhibit dose-dependent bone marrow suppression. More seriously, aplastic anaemia may rarely complicate chloramphenicol therapy. High doses of β-lactam antibiotics may induce granulocytopenia. Antibiotics are a rare cause of haemolytic anaemia. Many antibiotics cause a mild reversible thrombocytopenia or bone marrow depression.
Aminoglycosides may cause renal toxicity by damaging the cells of the proximal convoluted tubule. Patients who are elderly, have pre-existing renal disease or are also receiving other drugs with renal toxicity are at higher risk. Tetracyclines may also be toxic to the kidneys.
Liver
Isoniazid and rifampicin may cause hepatitis; this is more common in patients with pre-existing liver disease. Other agents associated with hepatitis are tetracycline, erythromycin, pyrazinamide, ethionamide and, very rarely, ampicillin or fluoroquinolones. Cholestatic jaundice may follow tetracycline or high-dose fusidic acid therapy.