Clostridium
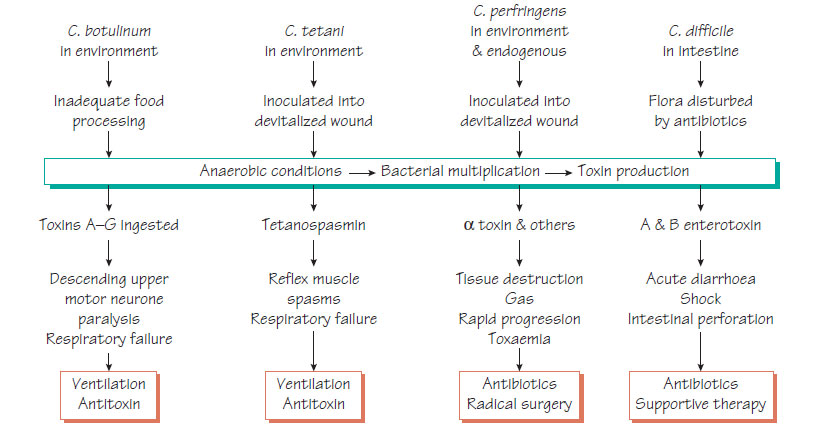
Clostridium spp. are anaerobic spore-forming organisms that are able to survive well in the environment. Their normal habitats are soil, water and the intestinal tract of humans and animals. Only a few of the 80 species are human pathogens. Toxin production is the main pathogenicity mechanism.Clostridium difficile
Pseudomembranous colitis, an acute inflammatory diarrhoeal disease, is an important cause of morbidity and mortality in hospitals.
The frequency of Clostridium difficile carriage increases with duration of hospital stay. When the gut microflora is disturbed by antibiotics overgrowth can occur. Enterotoxins A and B and binary toxin production cause tissue damage and fluid diarrhoea. Some strains that are fluoroquinolone resistant and have evidence of enhanced toxin production are associated with more severe disease and extensive hospital outbreaks.
Clinical features
- History of previous antibiotic exposure.
- Three or more loose/unformed stools per day.
- Possible development of abdominal pain.
- Pseudomembranes seen on sigmoidoscopy on the mucosal surface of the rectum and sigmoid colon.
- Possible complications of toxic megacolon, bowel perforation and systemic toxicity, which are associated with high mortality.
- Detection of toxin or glutamate dehydrogenase (GDH) by enzyme immunoassay (EIA).
- Detection of toxin genes by nucleic acid amplification test (NAAT).
- Typing - generally by ribotyping, but multilocus variablenumber tandem repeat analysis is superseding this.
Treatment and prevention
- Stop the inciting (antibiotic) agent.
- Treat with oral metronidazole for 10 days.
- Oral vancomycin plus intravenous metronidazole for severe cases and treatment failures.
- Relapse occurs in up to 25% of patients.
- Rapid and strict isolation is essential.
- Enhanced ward cleaning and attention to hand hygiene are essential (Awareness may be raised by 'SIGHT' - Suspect Isolate Gloves and aprons Hand hygiene Toxin test).
Clostridium botulinum is found in the environment and can contaminate wounds and food. Of the seven serotypes, A, B and E are most commonly associated with human disease.
Epidemiology and pathogenesis
Incomplete heat treatment of contaminated food in canning or bottling processes allows this organism to survive and produce toxin. Botulinum toxin, a neurotoxin, inhibits the release of neurotransmitters. Clinically, there are three forms of the disease: food intoxication, wound botulism and infant botulism.
Clinical features
- Rapid onset - within 6 h of ingestion.
- Descending flaccid paralysis, beginning with the cranial nerves.
- Dysphagia and blurred vision, followed by more general paralysis.
- Sensory function is normal.
- Infants appear floppy and listless, constipated and have generalized muscle weakness.
Diagnosis is based on the clinical features and a history of ingestion of suspect food. Toxin may be detected in food, faeces and serum by EIA. Botulinum neurotoxin genes can be detected by NAAT.
Treatment is with specific antitoxin and ventilatory support. Ventilator- associated pneumonia is an important complication. The disease is prevented by adequate process control in the foodprocessing industry and home preservation.
Gas gangrene
Clostridium perfringens is the organism most commonly associated with gas gangrene, but C. septicum, C. novyi, C. histolyticum and C. sordellii can also be implicated. C. perfringens is capsulate and produces a range of toxins, of which lecithinase C (a-toxin) is the most important.
Epidemiology and pathogenesis
- At-risk wounds are those where devitalized tissue is contaminated by environmental spores.
- Spores germinate and organisms multiply in the ischaemic conditions.
- Toxin is released.
- Toxin-mediated tissue damage creates more anaerobic conditions and progression is rapid.
- Infections can be mixed with other organisms especially in drug users.
Clinical features
- Onset within 3 days of injury.
- Pain in the wound.
- Tenseness of the skin, which develops an underlying blue discoloration, foul smell and crepitus.
- Toxaemia producing circulatory shock.
Diagnosis
Treatment and prevention
Treatment depends on debridement of devitalized tissue and intravenous antibiotics. Hyperbaric oxygen may also be beneficial. The condition is prevented by good management of potentially infected, devitalized wounds.
Clostridium perfringens food poisoning
This condition is typically associated with meals containing meat that are cooled slowly and subsequently reheated. Surviving clostridia release toxin in the stomach when they form spores; this leads to nausea, vomiting and diarrhoea. An EIA to detect toxin in faeces is available. Rarely, gut infection with clostridia causes severe enteritis.