Principles of infection control
Identifying an outbreakAn outbreak, whether in a hospital or the community, must first be recognized by clinical awareness and effective laboratory diagnosis; data must be managed centrally, a process usually described as surveillance.
Screening and diagnostics
It is necessary to make a laboratory diagnosis on patients with infection (e.g. to identify methicillin-resistant Staphylococcus aureus [MRSA] in the wounds of hospital patients, or influenza in patients in the community). The diagnostic methods, which are described in The laboratory investigation of infection , should be optimized to identify the organisms of concern. Precise diagnosis often requires the sample or organism to be sent to a reference laboratory. Identification of the organism should be sufficient to permit increased numbers of key pathogens to be recognized. For example, samples/organisms from patients with meningococcal disease should be confirmed and typed at the reference laboratory so that an increased incidence of infection with a particular strain can be detected.
Hospitals and communities require a mechanism to collate data as it emerges from laboratories, notifications and other systems, thus allowing an outbreak to be detected. This activity is performed locally by the hospital epidemiologist and nationally by epidemiologists in the public health service, which receives data from the reporting systems at reference laboratories and from other professionals such as environmental health officers.
Mandatory reporting and improvement targets with key measures have focused attention on healthcare-associated infections (e.g. MRSA and Clostridium difficile) and have proved beneficial in driving down infection rates.
Specific testing is used to identify the relationships between organisms: the more closely related organisms are, the more likely they are to have been transmitted from one person to another. Laboratory techniques should be simple to perform, reproducible and give identical results in all laboratories.
Laboratory testing can be divided into simple phenotypic testing and more complex molecular tests. Older methods such as serological and phage typing are being made obsolete by molecular methods.
Molecular typing involves the use of enzymes that can digest genomic, plasmid DNA or ribosomal RNA giving a pattern that can be compared between isolates. Identical organisms will have identical band patterns. Sequence-based methods are emerging, such as multilocus sequence typing (MLST) where a portion of seven housekeeping genes are sequenced to produce a numerical code for the organism. With reducing costs, sequencing of the whole genome may be used where variation is low and the importance of accuracy is high (e.g. a deliberate release of anthrax).
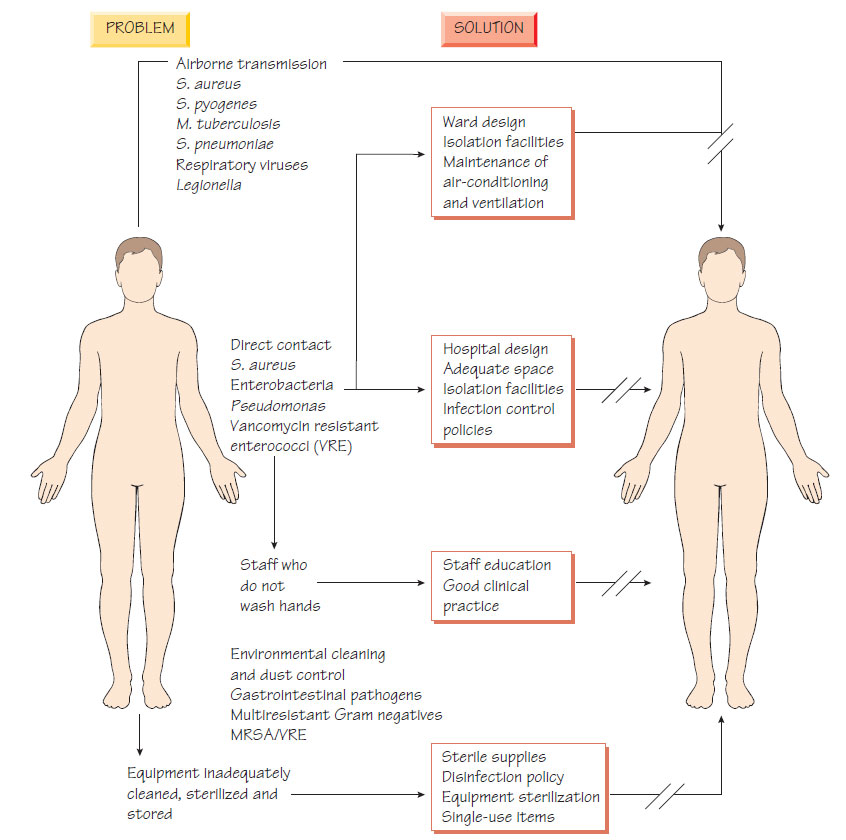
Infection can be controlled by separating infected patients from the uninfected before transmission occurs. Methods of achieving this will be detailed in the infection control policy. To be successful, this policy must be supported by the entire hospital staff. The control of infection team, which consists of a consultant infection specialist, management representation and specialist nurses, promotes the policy. The infection control committee must be linked to the senior hospital management committee. The team organizes hospital surveillance of high-risk organisms (e.g. MRSA) and must be involved in service development, including for example building alterations and new clinical services.
Isolation
Infected patients should be isolated (source isolation) using methods that will interrupt the means of transmission. Patients who are especially susceptible to infection require protective isolation.
For organisms spread by contact or by faecal-oral route, the following precautions should be taken:
- side-room isolation with dedicated hand-washing and toilet facilities;
- use of disposable plastic aprons and gloves for touching the patient;
- discarding of apron and gloves after use, then hand washing with liquid soap and disposable towels. Disinfection may reduce environmental contamination e.g. chlorine-containing agents for Clostridium difficile; see Clostridium).
Respiratory isolation
For organisms spread by the respiratory route, the following precautions should be taken:
- side-room isolation, as above;
- wearing of facemasks by staff/visitors when in the room;
- wearing of a facemask by the patient if transferred out of their room.
Strict isolation
This is used for patients with infections that carry a high mortality, such as viral haemorrhagic fevers (see Tropical, exotic or arbovirus infections). An enclosed isolation unit with negative-pressure and enclosed-air system, together with strict decontamination procedures, is used to prevent aerosol transmission of the organism.
Protective isolation is required for patients who are highly susceptible to infection, such those who are neutropenic as a result of radiotherapy or chemotherapy. The following procedures should be followed:
- side-room isolation;
- use of gloves and masks, as in wound and enteric infections;
- provision of filtered air;
- measures to control the risk from organisms in food (e.g. resistant Gram-negative organisms in vegetables or Listeria in soft cheeses).