Infections of the bones and joints
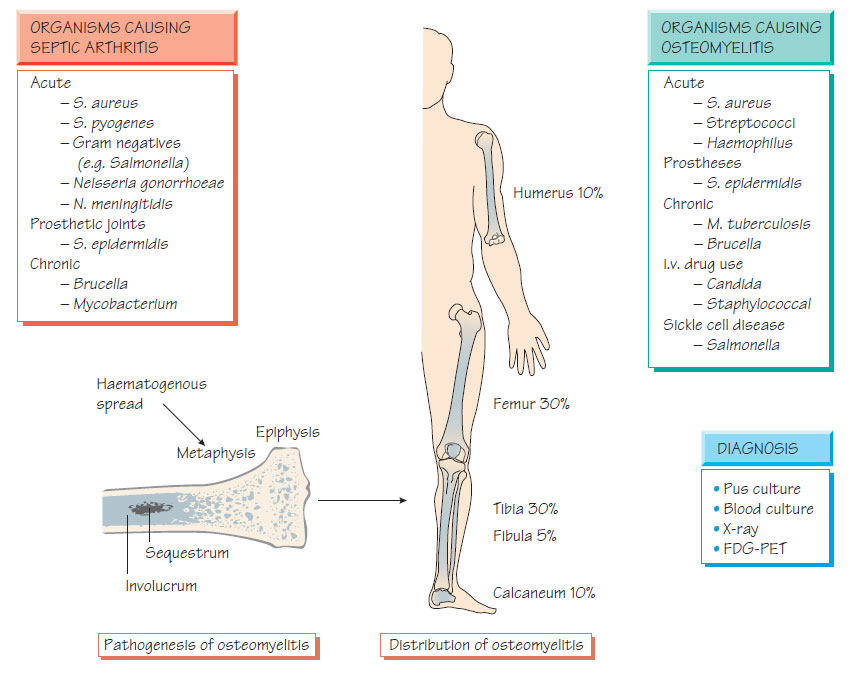
Osteomyelitis- Bone can be infected by haematogenous spread, by direct extension from an infected joint, or following trauma, surgery or instrumentation.
- The formation of pus precipitates ischaemia and necrosis; the central area of dead bone is known as the sequestrum.
- New bone (the involucrum) may form around the infection site.
- In children, the metaphysis of the long bones (femur, tibia and humerus) are most often involved. Infection of the spine is common in adults.
- Staphylococcus aureus accounts for 90% of infections; rarer causes includeStreptococcus pyogenes (4%), Haemophilus influenzae (4%), Escherichia coli, Salmonella spp., Mycobacterium tuberculosis and Brucella.
- Patients with sickle cell disease are especially prone to Salmonella infection.
- Presentation is with fever and pain. In the young, pain may be poorly localized but they may stop moving the affected limb (pseudoparalysis).
- Later, soft-tissue swelling may occur and can be followed by sinus formation.
- Pathological fractures may develop.
- Delayed treatment increases the risk of development of chronic osteomyelitis.
- Infection may develop around foreign bodies (e.g. surgical nails or debris from trauma).
Diagnosis
- Diagnosis is clinical.
- Radiological changes develop late in the course of infection and many not be seen.
- Isotope scans indicate sites of inflammation.
- Fluorodeoxyglucose positron emission tomography (FDGPET) is more sensitive.
- Blood cultures and pus from bone obtained via needle or open biopsy allow culture for pathogen identification and susceptibility testing.
- Drainage and excision of the sequestrum is supplemented by antibiotic therapy (e.g. flucloxacillin and fusidic acid pending culture results).
- If Salmonella is isolated or suspected, ciprofloxacin may be used.
- Treatment lasts for 6 weeks or until there is evidence that inflammation has disappeared and the bone has healed.
Chronic osteomyelitis
- Follows inadequately treated acute infection, or may be secondary to surgery or a fracture. Infection of prosthetic materials with organisms with reduced virulence, such as coagulase-negative staphylococci (CoNS) is increasingly common.
- S. aureus is implicated in 50% of cases; the remainder are associated with Gram-negative pathogens (e.g. Pseudomonas, Proteus and E. coli).
- On-going pain, swelling, deformity and/or a chronically discharging sinus may be found.
- Culture-based diagnosis is essential.
- A prolonged course of appropriate antibiotics should accompany appropriate surgery.
- Infected prosthetic devices are usually removed.
- Follows bacteraemia or injection of the joint.
- 95% of cases are caused by S. aureus and S. pyogenes. Other causes include Enterobacteriaceae, Neisseria gonorrhoeae, H. influenzae, Salmonella spp., Brucella spp., Borrelia burgdorferi, Pasteurella and M. tuberculosis.
- Large joints (e.g. the knee) are most commonly affected.
- Prosthetic joints are at risk of early and late infections (see below).
Clinical features
- Pain, swelling and reduced movement.
- In adults, the onset may be insidious; a history of recent urinary infection or salmonellosis may be reported.
- Cellulitis or specific signs, such as gonococcal rash may be found.
- Septic arthritis must be differentiated from acute rheumatoid arthritis, osteoarthritis, gout, pseudogout or reactive arthritis.
- A diagnostic tap will yield cloudy fluid, and Gram stain and white blood cell count may suggest infection that can be confirmed by culture or nucleic acid amplification test (NAAT).
- Culture for brucellosis should be performed if the history is suggestive.
Intravenous antibiotics that are appropriate to the infecting organisms, either isolated or suspected, should be commenced, and oral therapy is continued for up to 6 weeks. Aspiration and irrigation of the joint may be helpful in severe cases as it reduces inflammatory damage.
Some viruses are associated with arthritis, for example parvovirus, rubella, mumps and hepatitis B. Rubella-related arthritis is more common in females and develops a few days after the rash. Several of the alphaviruses cause severe bone and joint symptoms. Reactive arthritis caused by an immune response to the pathogen can follow recovery, for example after meningococcal disease, or Shigella or Chlamydia infection. The latter can be associated with uveitis and is known as Reiter's syndrome.
Prosthetic joint infections
Prosthetic joints may become infected at the time of operation (early presentation) or as a result of haematogenous spread (later presentation). In early presentation the organisms are from the skin (e.g. S. epidermidis and S. aureus including MRSA). Treatment is with intravenous antibiotics, depending on the susceptibility of the infecting organisms. Infection usually results in loss of the prosthesis. Prevention of infection by control measures in both the ward and theatre and antibiotic prophylaxis with an agent active against S. aureus (see Staphylococcus) is vital.