Infections of the central nervous system
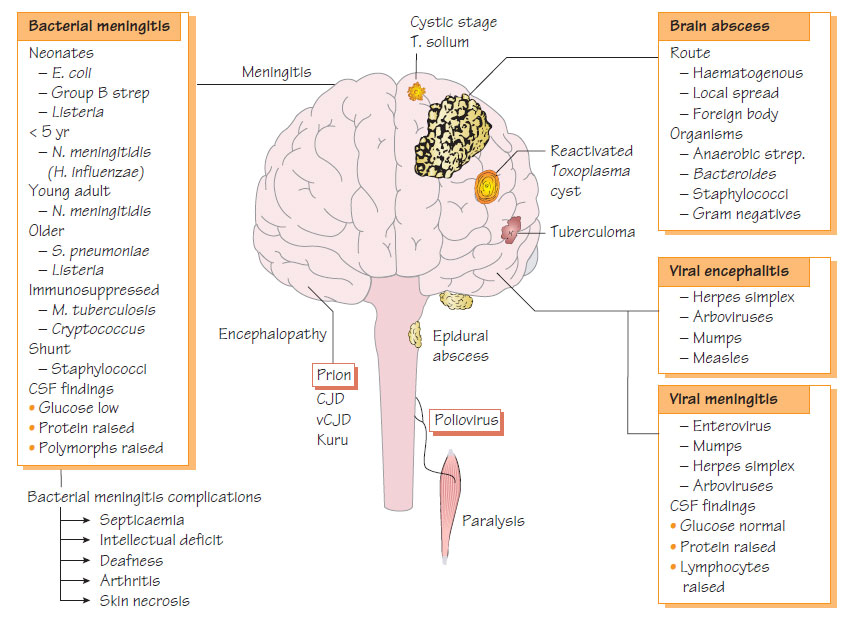
Bacterial meningitisClinical features
- Fever, headache, photophobia and neck stiffness.
- Occasionally vomiting and diarrhoea may predominate.
- Levels of consciousness fall progressively.
- Not all signs and symptoms may be present, especially in neonates and elderly people where presentation may be atypical.
- A bulging fontanelle in a neonate indicates raised intracranial pressure.
- Ear or sinus infections may suggest a pneumococcal cause.
- With appropriate treatment, mortality from Haemophilus influenzae and Neisseria meningitidis should be below 5%. However, N. meningitidis septicaemia can be rapidly fatal if the diagnosis is delayed.
- H. influenzae - recurrence of fever, hydrocephalus, convulsions and deafness.
- N. meningitidis - deafness, intellectual deficit, skin necrosis and reactive arthritis.
- Streptococcus pneumoniae has the highest mortality (>20%) and deafness, cranial nerve palsies and hydrocephalus are complications.
Diagnosis
- CSF should be obtained if possible but treatment of suspected meningitis should not be delayed.
- Total and differential white cell count, Gram stain, Ziehl- Neelsen, India ink, nucleic acid amplification test (NAAT) and antigen detection methods should be used.
- Blood should be taken for culture, rapid antigen detection and glucose determination. Meningococcal disease can be diagnosed by NAAT on whole blood.
- Neonatal meningitis (likely Escherichia coli, group B Streptococcus and Listeria): cefotaxime and an aminoglycoside, plus ampicillin if Listeria is suspected.
- Adult: ceftriaxone 2 g per day.
- If penicillin-resistant S. pneumoniae is suspected: vancomycin can be added.
- Cryptococcal meningitis: amphotericin and 5-flucytosine.
- Tuberculous meningitis: rifampicin, pyrazinamide, isoniazid and ethambutol (see Pathogenic mycobacteria).
- Shunt-related meningitis: treatment according to the identity and susceptibilities of the organisms.
Prevention
- Protein-conjugated polysaccharide vaccines are available for H. influenzae and N. meningitidis serogroups A and C, but not serogroup B, which causes most cases in the UK.
- Family (close) contacts of meningococcal and Haemophilus meningitis patients require antimicrobial prophylaxis (ciprofloxacin or rifampicin).
Brain abscesses arise from parameningeal suppuration, foreign bodies or haematogenous spread from distant sepsis. Infection is polymicrobial with anaerobic cocci, Prevotella spp., staphylococci, streptococci (S. anginosus/S. constellatus group) and Enterobacteriaceae.
Clinical features
- Headache, fever and reduced consciousness.
- Focal neurological signs depend on the location of the abscess.
- Signs of raised intracranial pressure may develop followed by seizures.
Diagnosis and Treatment
Lesions are localized by CT scanning. A lumbar puncture is contraindicated because of the risk of cerebellar herniation. Drainage should be performed if feasible and pus sent for culture, NAAT and sensitivity testing. A regimen of cefotaxime, metronidazole and penicillin or a combination of benzylpenicillin, chloramphenicol and metronidazole may be used.
Meningitis and encephalitis may arise from infection with enteroviruses, mumps, herpes simplex, arboviruses, influenza and, rarely, rubella or Epstein-Barr virus (EBV). Viral meningitis can be part of the natural history of polio infection (see Enterovirus and viruses that infect the gastrointestinal tract). Patients present with headache, photophobia, fever and neck stiffness. The CSF shows an increase in lymphocytes, a mildly raised protein level and normal glucose level. Throat swabs, CSF and stool specimens should be sent for NAAT and serological testing. management is symptomatic as most patients recover without residual deficit within a few days.
Viral encephalitis
Viral encephalitis is caused by a variety of viruses including herpesvirus and arbovirus (see Herpesviruses II and Tropical, exotic or arbovirus infections). Patients are febrile with headache, neck stiffness and impaired consciousness. Focal neurological signs may develop; convulsions are common. Virus may be detected in CSF, stool and throat specimens by NAAT and serological techniques. Aciclovir is used for Treatment of herpetic encephalitis and has led to reductions in both mortality and the number of patients left with severe residual disability.
Some viruses are associated with encephalitis after a systemic infection has resolved, known as postinfectious encephalitis (e.g. measles, varicella zoster, rubella, EBV, mumps and influenza). Clinically similar to viral meningitis, this condition is thought to be mediated by an autoimmune reaction.
Spongiform encephalopathies
The prion protein is a protease-resistant form of a protein that is a normal constituent of the brain. When ingested, the prion protein induces a conformational change in the host brain protein, which leads to spongiform degeneration in the brain. There is an extended incubation period of more than 5 years. Kuru was a disease seen in Papua New Guinea among people who ate human tissue, including brain. Variant Creutzfeldt-Jakob disease (vCJD) arose after animal brain protein was fed to cattle, the disease being transmitted to humans by ingestion of contaminated beef products. The animal disease, bovine spongiform encephalopathy (BSE), has been eliminated in countries with effective control measures. The size and scale of any human epidemic is uncertain but likely to be small.