Respiratory tract infections
Upper respiratory tract infectionsPharyngitis
This is a common condition seen in community practice. Patients have fever and a painful, infected throat that may have visible pus or exudate. Regional lymph nodes may be painful and enlarged. Bacterial and fungal causes includeStreptococcus pyogenes, Neisseria gonorrhoeae and Candida. Corynebacterium diphtheriae infection should be considered if there is an appropriate travel or vaccination history (see Immunization). Streptococcal infection may be complicated by peritonsillar abscess (quinsy), bacteraemia, rheumatic fever or nephritis.
- Most infections in adults are viral so symptomatic treatment is usually adequate.
- Penicillin V or a macrolide is given if bacterial infection is suspected or proven by near-patient testing.
- Ampicillin should be avoided as it may provoke a rash with Epstein-Barr virus (EBV) infection.
- Tonsillectomy or adenoidectomy may reduce the frequency of episodes of pharyngitis or otitis media in patients with quinsy or recurrent otitis media.
Otitis media and sinusitis
- Infection occurs when the Eustachian tube or sinuses are occluded by inflammation.
- Children under 7 years are especially prone because the Eustachian tube is short, narrow and nearly horizontal.
- Streptococcus pneumoniae, S. pyogenes, Haemophilus influenzae, Moraxella catarrhalis and the more recently recognized Alloiococcus otitidis are the commonest causative organisms.
- Presentation is with local pain and fever.
- With sinusitis, the pain may be worse with head movement and in the evening.
- Ear infection may be complicated by perforation, recurrent or chronic infection or the development of 'glue ear' (sterile mucus within the middle ear).
- Rarely, acute meningitis or mastoiditis can complicate severe infection.
- Diagnosis is clinical: an auroscope may show retrotympanic fluid levels, an inflamed tympanic membrane or a purulent discharge associated with perforation.
- Treatment depends on reducing the mucosal swelling, promoting drainage of the fluid and encouraging the recirculation of air.
- Appropriate antibiotic therapy is used in more severe cases.
This infectious swelling of the epiglottis may threaten the airway. H. influenzae type b was a common cause until vaccination became available. Infection with S. pyogenes causes some cases, usually in adults.
- Presentation is with sore throat and high fever.
- Stridor and drooling are usually present.
- Throat examination should be avoided because it may precipitate acute respiratory obstruction.
- Treatment is with parenteral third-generation cephalosporins.
- Emergency tracheostomy may become necessary.
Epidemiology
Infections of the lower respiratory tract are an important cause of morbidity and mortality worldwide and a major cause of death in children under 5 years. Predisposing factors include:
- smoking;
- chronic obstructive pulmonary disease;
- diabetes mellitus;
- immunosuppressive therapy;
- HIV.
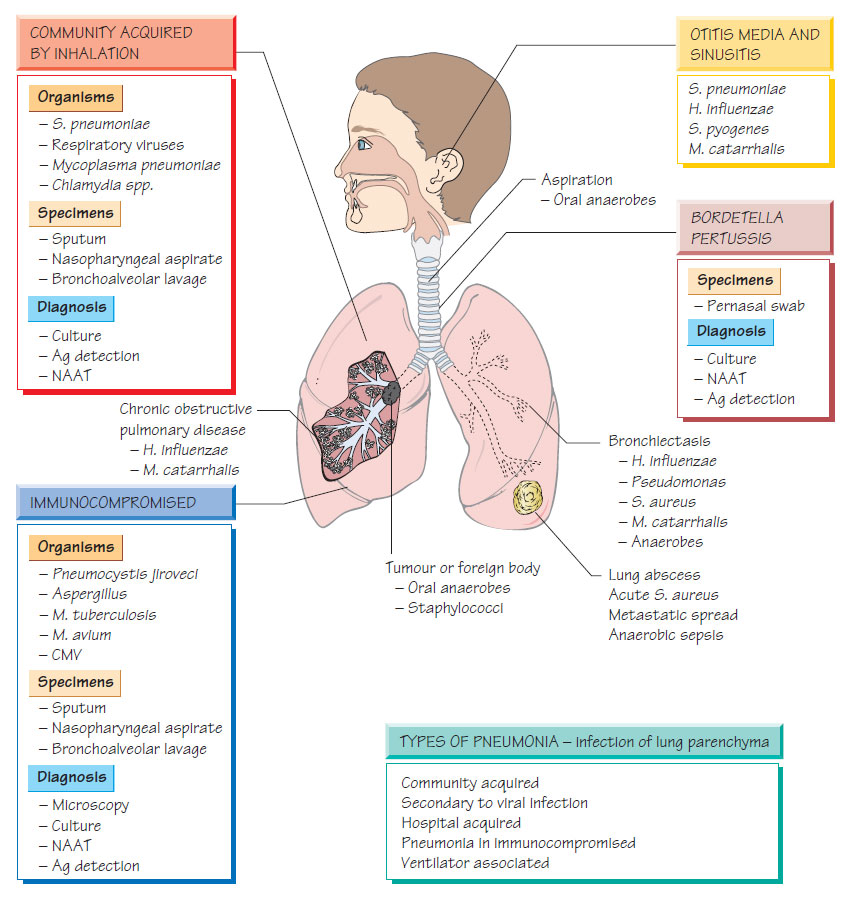
The bacterial causes are illustrated and many viruses cause primary viral pneumonia (e.g. influenza and SARS coronavirus). Others cause damage to the lower respiratory tract, permitting secondary bacterial pneumonia.
- Fever and a cough.
- Purulent sputum production that may be blood stained.
- Some pathogens (e.g. Mycoplasma) rarely cause productive cough.
- Pleural inflammation causes sharp chest pain that is worse on inspiration.
- Signs of systemic infection, such as myalgia, malaise and weakness, may be present.
- In elderly people, mental confusion is common even when specific symptoms and signs are slight.
Complications
- Pleural and pericardial spread.
- Septicaemia.
- Meningitis.
- Staphylococcus aureus infection can be complicated by lung cavitation and bronchiectasis.
Diagnosis
Diagnostic samples include:
- expectorated sputum;
- induced sputum;
- bronchoalveolar lavage (especially for suspected tuberculosis or for immunocompromised patients).
Rapid diagnostic techniques may be possible, such as urinary antigen detection for S. pneumoniae and Legionella pneumophila) Multiplex nucleic acid amplification tests (NAATs) are available for all respiratory pathogens and can be performed quickly enough to inform treatment choice.
- Appropriate antibiotic therapy should be started as soon as possible.
- Severe, community-acquired pneumonia requires hospitalization with intravenous antibiotics (e.g. a third-generation cephalosporin and macrolide).
- Milder infections can be treated with oral therapy, often with amoxicillin and/or a macrolide, although quinolones such as moxifloxacin are also used. As β-lactam resistance is common in H. influenzae, patients with chronic obstructive pulmonary disease should be treated with an appropriate agent (e.g. co-amoxiclav or trimethoprim).
- Treatment of hospital-acquired pneumonia may require agents that are active against Enterobacteriaceae and Pseudomonas (e.g. ciprofloxacin or ceftazidime).
- Supportive therapy may include bed-rest, oxygen, rehydration, physiotherapy and ventilation if needed.