The Menstrual Cycle
The Menstrual Cycle
The human menstrual cycle (L. mensis,
month) consists of two distinct phases
within the ovary: follicular phase and
luteal phase, and three distinct phases
within the uterus: menstrual phase, proliferative
phase and secretory phase
(Figure 7-15). Menstruation (the
“period”) signals the menstrual phase, when part of the lining of the uterus
(endometrium) degenerates and
sloughs off, producing the menstrual
discharge. Meanwhile, the follicular
phase within the ovary is occurring,
and by day 3 of the cycle blood levels
of FSH and LH begin to rise slowly,
prompting some of the ovarian follicles
to begin growing and to secrete estrogen.
As estrogen levels in the blood
increase, the uterine endometrium heals
and begins to thicken, and uterine
glands within the endometrium enlarge
(proliferative phase). By day 10 most
of the ovarian follicles that began to
develop at day 3 now degenerate
(become atretic), leaving only one
(sometimes two or three) to continue
ripening until it appears like a blister on
the surface of the ovary. This is a
mature follicle or graafian follicle.
During the latter part of the follicular
phase, the graafian follicle secretes
more estrogen, and also inhibin. Inhibin
acts as a negative feedback regulator of
FSH (as in males), and as the levels of
inhibin rise, the levels of FSH fall.
At day 13 or 14 in the cycle, the now high levels of estrogen from the graafian follicle stimulate a surge of GnRH from the hypothalamus, which induces a surge of LH (and to a lesser extent, FSH) from the anterior pituitary. The LH surge causes the largest follicle to rupture (ovulation), releasing the oocyte from the ovary. Now follows a critical period, for unless a mature oocyte is fertilized within a few hours, it will die. During the ovarian luteal phase, a corpus luteum (“yellow body” for its appearance in cow ovaries) forms from the remains of the ruptured follicle that released the oocyte at ovulation (Figures 7-10 and 7-15). The corpus luteum, responding to continued stimulation of LH, becomes a transitory endocrine gland that secretes progesterone (and estrogen in primates). Progesterone (“before carrying [gestation]”), as its name implies, stimulates the uterus to undergo final maturational changes that prepare it for gestation (secretory phase). The uterus is now fully ready to house and nourish an embryo. If fertilization has not occurred, the corpus luteum degenerates, and its hormones are no longer secreted. Since the uterine lining (endometrium) depends on progesterone and estrogen for its maintenance, their declining levels cause the uterine lining to deteriorate, leading to menstrual discharge of the next cycle.
Oral contraceptives (the “pill”) usually are combined preparations of estrogen and progesterone that act to decrease the output of pituitary gonadotropins FSH and LH. This prevents the ovarian follicles from ripening and ovulation from occurring. Oral contraceptives are highly effective, with a failure rate of less than 1% if the treatment procedure is followed properly.
GnRH from the hypothalamus, and LH and FSH from the anterior pituitary, are controlled by negative feedback of ovarian steroids (and inhibin). This negative feedback occurs throughout the menstrual cycle, except for a few days before ovulation. As mentioned above, ovulation is due to the high levels of estrogen causing a surge of GnRH, LH (and FSH). Such positive feedback mechanisms are rare in the body, since they move events away from stable set points. This event is terminated by ovulation when estrogen levels fall as an oocyte is released from the follicle. (See Chemical Coordination) for more information on negative and positive feedback mechanisms.)
While women in more than 90 other countries benefit from safe, recently-developed, easier-to-use contraceptives, American couples have until recently been limited to the standby contraceptives developed more than 30 years ago: the Pill, condom, IUD, diaphragm, and surgical sterilization. Progesterone- only methods of contraception have more recently been made available in this country, including the “mini-pill,”Depo- Provera and Norplant. Contraception for men (other than condoms) is still unavailable. The new contraceptive additions have significantly reduced the risk of unwanted pregnancies, but the cost of contraception is often prohibitive and it is not made available to younger, sexually active individuals. An unfortunate consequence is that lack of use of contraception, together with contraceptive failures, account for some 2 million unwanted pregnancies each year in the United States and for about half the 1.5 million abortions, one of the highest abortion rates in the industrialized world.Without a change in the present adverse policies, there is little hope of reducing unwanted pregnancies.
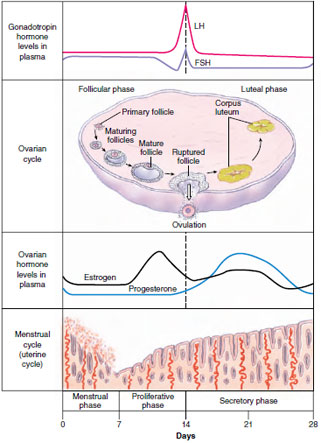 |
| Figure 7-15 Human menstrual cycle, showing changes in blood hormone levels and uterine endometrium during the 28-day cycle. FSH promotes maturation of ovarian egg follicles, which secrete estrogen. Estrogen prepares the uterine endometrium and causes a surge in LH, which in turn stimulates the corpus luteum to secrete progesterone and estrogen. Progesterone and estrogen production will persist only if the egg is fertilized; without pregnancy progesterone and estrogen levels decline and menstruation follows. |
At day 13 or 14 in the cycle, the now high levels of estrogen from the graafian follicle stimulate a surge of GnRH from the hypothalamus, which induces a surge of LH (and to a lesser extent, FSH) from the anterior pituitary. The LH surge causes the largest follicle to rupture (ovulation), releasing the oocyte from the ovary. Now follows a critical period, for unless a mature oocyte is fertilized within a few hours, it will die. During the ovarian luteal phase, a corpus luteum (“yellow body” for its appearance in cow ovaries) forms from the remains of the ruptured follicle that released the oocyte at ovulation (Figures 7-10 and 7-15). The corpus luteum, responding to continued stimulation of LH, becomes a transitory endocrine gland that secretes progesterone (and estrogen in primates). Progesterone (“before carrying [gestation]”), as its name implies, stimulates the uterus to undergo final maturational changes that prepare it for gestation (secretory phase). The uterus is now fully ready to house and nourish an embryo. If fertilization has not occurred, the corpus luteum degenerates, and its hormones are no longer secreted. Since the uterine lining (endometrium) depends on progesterone and estrogen for its maintenance, their declining levels cause the uterine lining to deteriorate, leading to menstrual discharge of the next cycle.
Oral contraceptives (the “pill”) usually are combined preparations of estrogen and progesterone that act to decrease the output of pituitary gonadotropins FSH and LH. This prevents the ovarian follicles from ripening and ovulation from occurring. Oral contraceptives are highly effective, with a failure rate of less than 1% if the treatment procedure is followed properly.
GnRH from the hypothalamus, and LH and FSH from the anterior pituitary, are controlled by negative feedback of ovarian steroids (and inhibin). This negative feedback occurs throughout the menstrual cycle, except for a few days before ovulation. As mentioned above, ovulation is due to the high levels of estrogen causing a surge of GnRH, LH (and FSH). Such positive feedback mechanisms are rare in the body, since they move events away from stable set points. This event is terminated by ovulation when estrogen levels fall as an oocyte is released from the follicle. (See Chemical Coordination) for more information on negative and positive feedback mechanisms.)
While women in more than 90 other countries benefit from safe, recently-developed, easier-to-use contraceptives, American couples have until recently been limited to the standby contraceptives developed more than 30 years ago: the Pill, condom, IUD, diaphragm, and surgical sterilization. Progesterone- only methods of contraception have more recently been made available in this country, including the “mini-pill,”Depo- Provera and Norplant. Contraception for men (other than condoms) is still unavailable. The new contraceptive additions have significantly reduced the risk of unwanted pregnancies, but the cost of contraception is often prohibitive and it is not made available to younger, sexually active individuals. An unfortunate consequence is that lack of use of contraception, together with contraceptive failures, account for some 2 million unwanted pregnancies each year in the United States and for about half the 1.5 million abortions, one of the highest abortion rates in the industrialized world.Without a change in the present adverse policies, there is little hope of reducing unwanted pregnancies.




