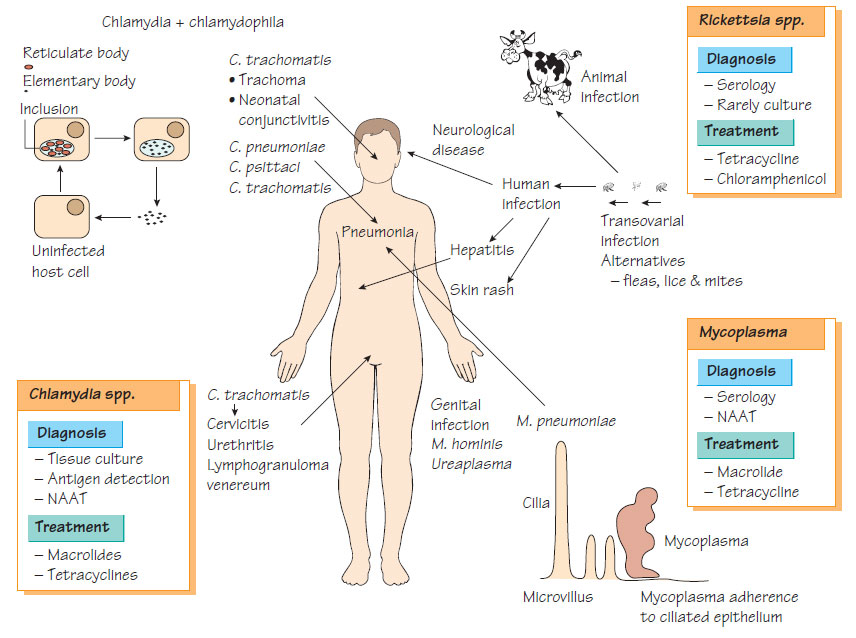
Chlamydia, Mycoplasma and Rickettsia
ChlamydiaThere are three species: Chlamydia trachomatis, which infects the eye and the genital tract; and two respiratory pathogens, C. pneumonia and a related species Chlamydophila psittaci. They are obligate, intracellular bacteria that exist in two forms: the reticulate body (a non-infective, intracellular, vegetative form) and the elementary body (an extracellular form that permits the organism to survive and be transmitted), which is derived from the reticulate body by binary fission.
Pathogenicity
The major outer membrane protein may participate in attachment to mucosal cells. A 60-kDa cysteine-rich protein may also be associated with virulence.
Chlamydia pneumoniae is transmitted from person to person by the respiratory route. It produces pneumonia or bronchitis, which is usually clinically mild, but may be associated with pharyngitis, sinusitis and laryngitis.
Chlamydia trachomatis
There are multiple serotypes of C. trachomatis: A-C are associated with trachoma (see Ocular infections) and neonatal conjunctivitis (see Congenital and perinatal infections); D-K are associated with acute urethritis and pelvic inflammatory disease (see Urinary and genital infections); serotypes L1-L3 are associated with lymphogranuloma venereum (see Urinary and genital infections).
Chlamydophila psittaci
Chlamydophila psittaci, a pathogen of birds and mammals, causes psittacosis in humans. After an incubation period of 10-14 days, fever, a dry unproductive cough, dyspnoea, headache and myalgia develop. Clinical examination reveals few signs of consolidation, but chest X-ray may show patchy consolidation.
- For C. trachomatis, usually by nucleic acid amplification test (NAAT) although enzyme immunoassay (EIA) and culture are available.
- For C. pneumoniae, usually by NAAT or serology.
- Psittacosis is usually diagnosed serologically.
Mycoplasma and Ureaplasma
Mycoplasma and Ureaplasma are small bacteria that lack a cell wall.
- Mycoplasma pneumoniae, a human respiratory pathogen, is the second most common cause of respiratory infection after Streptococcus pneumoniae.
- Mycoplasma hominis and Ureaplasma urealyticum have uncertain roles in relation to genital infection.
- Mycoplasma genitalium may be associated with urethritis.
Pathogenicity
Mycoplasma pneumoniae adheres to host cells by the P1 protein, localizing to the base of the cilia where it induces ciliostasis. Secreted hydrogen peroxide damages host membranes and interferes with superoxide dismutase and catalase. Opsonized M. pneumoniae is readily killed by macrophages and by the activity of the complement system.
Patients present with fever, myalgia, pleuritic chest pain and a non-productive cough; headache is a prominent symptom. Antibodies that agglutinate the host's red blood cells at low temperature (cold agglutinins) cause peripheral and central cyanosis. Infection is associated with reactive (postinfective) arthritis, and neuritis.
Laboratory Diagnosis
NAAT is the method of choice for all Mycoplasma spp., although serology is an alternative.
Treatment
- They are sensitive to erythromycin, tetracycline, aminoglycosides, rifampicin, chloramphenicol and quinolones.
- They are resistant to β-lactams.
These organisms are obligate intracellular bacteria with biochemical similarities to Gram-negative bacteria. Clinically, they are divided into three groups: 1 spotted fever; 2 scrub typhus; 3 typhus. Spotted fever is generally transmitted by ticks. Scrub typhus is caused by a single species, Rickettsia tsutsugamushi. The typhus group includes R. prowazekii and R. typhi, which cause epidemic and murine typhus respectively. Typical features include:
- a 14-day incubation period;
- initial non-specific symptoms, which are followed by possible development of fever, arthralgia and malaise, then a rash, conjunctivitis and pharyngitis;
- confusion, which occurs only in a proportion of Rocky Mountain Spotted Fever cases;
- relapse of R. prowazekii infection months or years later, which is known as Brill-Zinsser disease and is usually milder than the primary infection;
Diagnosis is usually by NAAT or IgM-specific EIA. Tetracyclines and chloramphenicol are the treatments of choice, but must be initiated early to influence the outcome.
Coxiella burnetii is a pathogen of cattle, sheep and goats, which localizes in the placenta. It survives desiccation in the environment and is transmitted by contact with infected animals or their products via the aerosol route. Typical features include:
- an acute febrile illness with fever, myalgia and cough;
- a chronic infection, which occurs in approximately 5% of cases;
- Q fever, which may present as atypical pneumonia, pyrexia of uncertain origin and hepatitis.
- various complications including relapses, which can take the form of culture-negative endocarditis or granulomatous hepatitis.