Environmental pathogens: Pseudomonas, Burkholderia and Legionella
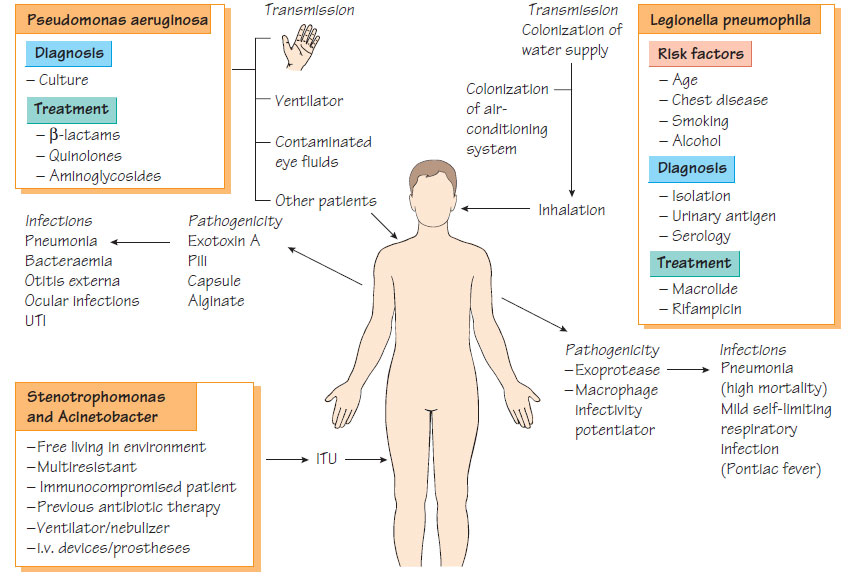
Pseudomonas spp.Most Pseudomonas spp. are environmental organisms that can cause opportunistic infections in a healthcare environment.
Pseudomonas aeruginosa
This organism is widespread in the environment, but rare in the flora of healthy individuals. Its carriage increases with hospitalization. Moist places such as sink-traps, drains and flower vases can harbour Pseudomonas.
Pathogenesis
- Produces cytotoxins and proteases (e.g. exotoxins A and S, haemolysins and elastase).
- Isolates from patients with cystic fibrosis produce a polysaccharide alginate that protects from opsonization, phagocytosis and antibiotics in microcolonies.
- Alginate, pili and outer membrane protein mediate adherence.
- Alginate production is associated with hypersusceptibility to antibiotics, lipopolysaccharide deficiency, non-motility and reduced exotoxin production.
- Chronic pulmonary infection in cystic fibrosis.
- Septicaemia, which has a high mortality and is a particular threat to neutropenic patients.
- Rapidly progressive corneal infection and otitis externa.
- Colonization of burns, followed by septicaemia.
- Ecthyma gangrenosum, a destructive skin complication of bacteraemia.
- Osteomyelitis, septic arthritis and meningitis.
Laboratory Diagnosis
- Culture on selective media containing cetrimide, irgasin and naladixic acid.
- Identification by biochemical testing.
- Typing by pulse-field gel electrophoresis or multilocus sequence typing (MLST).
Treatment
Organisms are often resistant; therefore, treatment is guided by susceptibilities.
Despite active research there is no effective vaccine available; transmission of multiresistant strains should be controlled by the methods described in Infection in the hospital environment.
Burkholderia spp.
Burkholderia cepacia
- This organism can cause chronic pulmonary infection among patients with cystic fibrosis.
- It can spread from patient to patient in cystic fibrosis clinics.
- It is naturally resistant to many antibiotics.
- Treatment is based on susceptibility tests and may include expandedspectrum cephalosporins, carbapenems or ureidopenicillins.
Burkholderia pseudomallei
This organism is found in soil and water in the tropics. It causes melioidosis that may present as a tuberculosis-like disease, as acute septicaemia or as multiple abscesses. Septicaemia is associated with a high mortality. The diagnosis is made by cultivating the organism from blood or tissues. Treatment is with ceftazidime or imipenem. B. mallei causes a similar infection in horses, known as glanders, which can spread to humans.
These organisms are found in moist environments, are naturally resistant to many antibiotics and can colonize patients who are immunocompromised or in intensive care units Infection is transmitted by staff or by contaminated shared equipment, such as nebulizers, and is more likely to occur in patients who are receiving antibiotics, have multiple cannulae or are intubated. Both organisms have been implicated in outbreaks of multidrug-resistant infection and systemic invasion leads to pneumonia, septicaemia, meningitis or urinary tract infection. Treatment, when indicated, is based on the results of susceptibility tests.
- There are more than 39 species of Legionella, but L. pneumophila is most frequently implicated in human disease.
- They are found in rivers, lakes, warm springs, domestic watersupplies, fountains, air-conditioning systems, swimming pools and jacuzzis.
- Multiplication occurs at temperatures between 20 and 40°C inside Acanthamoeba.
- Transmission is via aerosols generated from, for example, showers and air-conditioning systems.
- Infection is associated with previous lung disease, smoking and high alcohol intake, but previously healthy patients can be infected.
- Immunocompromised patients in hospital are vulnerable to infection if the hospital air-conditioning system is not adequately maintained.
- A major outer membrane protein that inhibits acidification of the phagolysosome.
- Macrophage infectivity is required for optimal internalization.
- L. pneumophila expresses a potent exoprotease.
Clinical features
- A mild, influenza-like illness (Pontiac fever).
- Severe pneumonia (Legionnaires' disease), which can lead to respiratory failure and high mortality.
- Patients may complain of nausea or vomiting and malaise before lung symptoms become prominent.
- Cough, which is usually unproductive, and dyspnoea, which is progressive.
- Confusion is common.
- Inappropriate naturetic hormone production may be associated with low serum sodium.
- Culture of sputum or, preferably, bronchoalveolar lavage fluid.
- Rapid diagnosis by antigen detection in urine.
- Direct immunofluorescence or nucleic acid amplification test (NAAT) of respiratory specimens.
- Serum antibodies can provide a retrospective diagnosis for epidemiological purposes.
Treatment and Prevention
Effective regimens usually consist of a macrolide antibiotic together with rifampicin. Legionellosis is prevented by adequate maintenance of air-conditioning systems and by ensuring that hot-water supplies are above 45°C to prevent multiplication.