Spiral bacteria
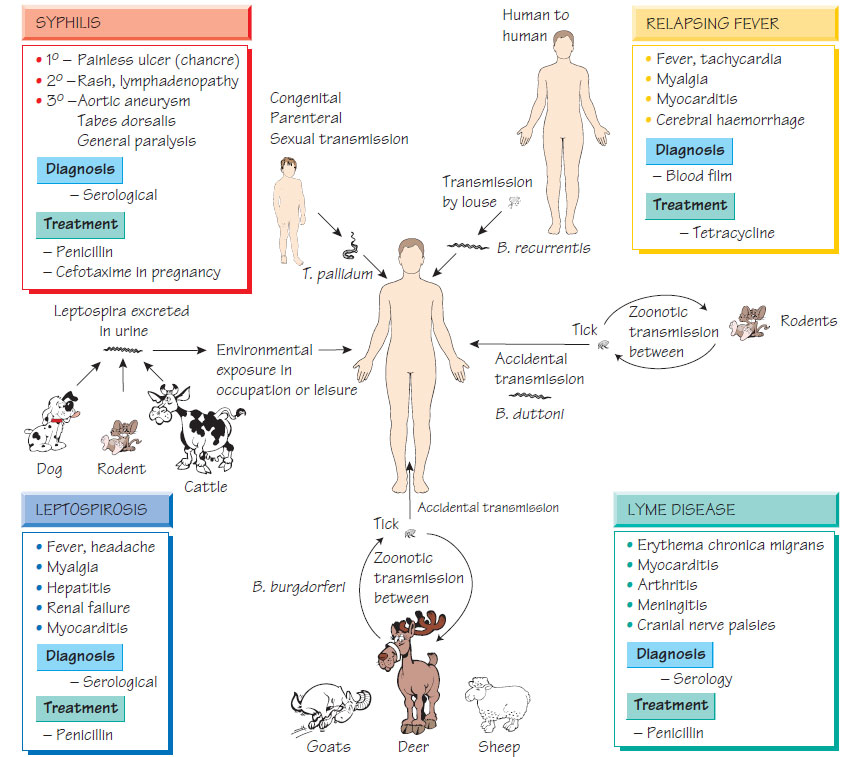
LeptospiraThere are two main species: Leptospira interrogans, which contains all of the pathogenic strains, and L. biflexa, a non-pathogen. L. interrogans has more than 200 serovariants that may be written as if they are separate species.
Epidemiology
Leptospira interrogans have different preferred mammalian hosts, for example the rat is the reservoir of L. interrogans Icterohaemorrhagiae. Leptospires colonize the renal tubules of their natural hosts and are excreted in urine. Humans may be infected by contact with animal urine or contaminated water or soil. Watersports enthusiasts, sewer workers and agricultural workers are at increased risk of infection.
The central nervous system, liver and kidneys are most affected by the human disease. The severity varies between serovars. There are two phases:
- bacteraemia, with fever, headache, myalgia, conjunctivitis and abdominal pain;
- fever, uveitis and aseptic meningitis, which predominate after the organisms disappear from the blood.
Borrelia are transmitted to humans via arthropods (lice or ticks) throughout the world, with a well-defined geographical territory and host specificity. For example, humans are the only host of louse-borne relapsing fever (B. recurrentis). Epidemics arise during war or mass migration when humans invade the Borrelia-tick- rodent habitat.
Relapsing fever
- Borrelia cause bacteraemia and fever. Antibodies clear the organism from the blood, but antigenic variation allows relapse. The disease resolves when the repertoire of antigenic variation is exhausted.
- Presentation is with headache, myalgia, tachycardia, rigors, hepatosplenomegaly and a petechial rash.
- Episodes last for 3-6 days; relapses occur a week apart.
- Louse-borne relapsing fever has a high mortality (up to 40%); mortality in tick-borne disease rarely exceeds 5%.
- Myocarditis, cerebral haemorrhage and/or hepatic failure are the usual causes of death.
- Postexposure doxycycline is effective in preventing disease.
- Doxycycline is treatment of choice.
Borrelia burgdorferi, B. afzelii and B. garinii are transmitted by Ixodes ticks and cause Lyme disease, which is endemic in the eastern USA and Europe. Humans are accidental hosts. The early symptoms are caused by the acute infective process; later manifestations are thought to be related to the host immune response. Typical features include:
- an initial expanding red macule or papule (erythema chronicum migrans);
- later headache, conjunctivitis, fever and regional lymphadenopathy;
- complications including new skin lesions, myocarditis, arthritis, aseptic meningitis, cranial nerve palsies and radiculitis;
- acrodermatitis chronica atrophicans, a red skin lesion, which may also occur.
Diagnosis is made by EIA followed by Western blot. Doxycycline or amoxicillin is used for treatment of early Lyme disease; ceftriaxone for late or recurrent disease.
This is a painful, oral, ulcerative, destructive infection with Borrelia vincentii and fusobacteria or other anaerobes. Clinical diagnosis is confirmed by Gram stain. Treatment is with penicillin and metronidazole.
Treponema pallidum
Treponema pallidum causes syphilis, which may be transmitted sexually or congenitally. The incidence is now increasing worldwide, having been falling for many years. The related organisms T. pertenue and T. carateum cause yaws and pinta respectively. They are spread by contact, usually in childhood. Once common in the tropics, they are now rare as the result of an eradication campaign.
Treponema pallidum penetrate intact skin or mucosa disseminating throughout the body to cause disease in four stages:
- Primary chancre (painless ulcer with a rubbery edge and regional lymphadenopathy).
- Secondary (an acute febrile illness with a generalized non-itchy scaling rash that typically involves the palms, associated with lymphadenopathy).
- Latent phase, which may last for many years.
- Tertiary (systemic lesions become symptomatic, e.g. aortitis, posterior cord degeneration and dementia).
The characteristic syphilitic lesions (gummas), which consist of necrosis and obliterative endarteritis with fibroblastic proliferation and lymphocyte infiltration, are found throughout the body.
Diagnosis
- Primary: dark-ground microscopy or NAAT.
- Later stages: EIA for specific IgG and IgM as well as cardiolipin agglutination (measures disease activity) and tests based on cultivated treponemes such as the treponemal haemagglutination test (TPHA).
- CSF testing should be performed to detect early central nervous system involvement.
- Neonatal: detection of IgM by Western blotting.
- Penicillin (or either azithromycin or tetracyclines if the patient is allergic).
- An acute febrile response (the Jarisch-Herxheimer reaction) may develop in some patients after the first dose of antibiotics.
- Careful serological follow-up is essential to confirm cure and/or detect early central nervous system involvement.