Small Gram-negative coccobacilli:Haemophilus, Brucella, Francisella, Yersinia, Bartonella
HaemophilusHaemophilus spp. are fastidious Gram-negative coccobacilli that colonize mucosal surfaces. H. influenzae and H. ducreyi are the main pathogenic species.
Haemophilus influenzae
Haemophilus influenzae expresses an antiphagocytic polysaccharide capsule of which there are six types (a-f). It also expresses a lipopolysaccharide (LPS) and an IgA1 protease. Septicaemia, meningitis and osteomyelitis are usually associated with type b infection in individuals who have not been vaccinated.
Infection occurs in preschool children, causing pyogenic meningitis, acute epiglottitis, septicaemia, facial cellulitis or osteomyelitis. Non-capsulate strains are usually commensal in the nasopharynx, but may cause adult otitis media, sinusitis, and chest infection in patients with obstructive airways disease.
Laboratory Diagnosis
Antigen detection provides rapid diagnosis in meningitis. Culture of CSF, sputum, blood or pus is used. Increasingly, H. influenzae is diagnosed as part of multiplex nucleic acid amplification tests (NAATs).
Treatment and Prevention
Many H. influenzae express a β-lactamase and are ampicillin resistant. Co-amoxiclav, clarithromycin, tetracycline or trimethoprim can be used. Severe infections are treated with a β-lactam-stable cephalosporin. A protein-conjugated polysaccharide vaccine against type b has almost eradicated childhood infection. Non-capsulate Haemophilus is ubiquitous and predisposed patients cannot avoid infection.
Haemophilus ducreyi is transmitted sexually and causes painful, irregular, soft genital ulcers (chancroid). There is associated lymphadenopathy, and suppurating inguinal lymph nodes may lead to sinus formation. Infection is more common in developing countries and facilitates the transmission of HIV. Transmission is controlled by treatment with azithromycin, ceftriaxone or a fluoroquinolone coupled with efficient contact tracing (see Sources and transmission of infection).
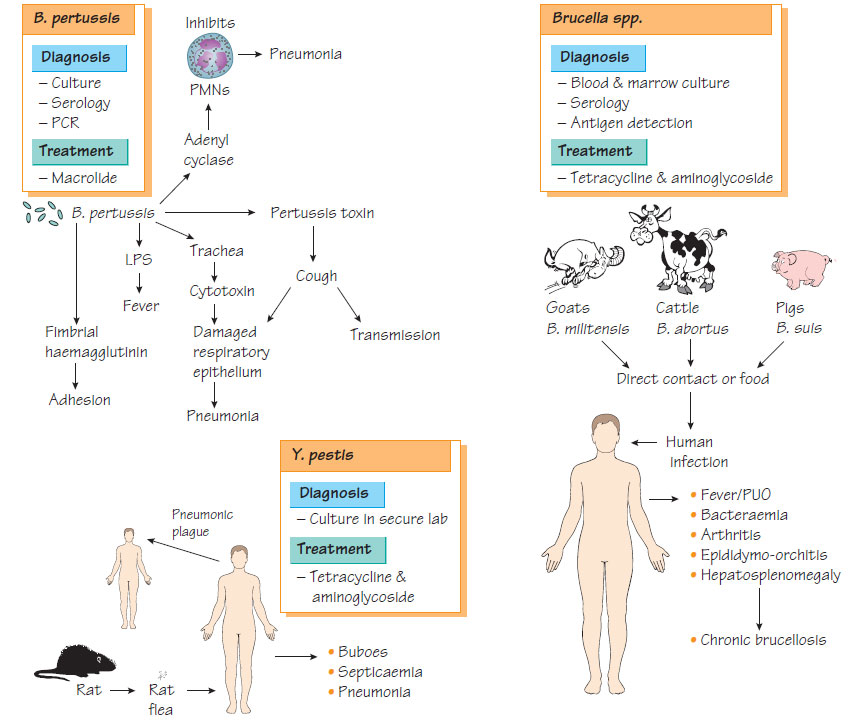
Brucella spp.
Brucella melitensis, B. abortus and B. suis have goats, cattle and pigs, respectively, as their main hosts. They are aerobic or capnophilic and require serum-containing medium to grow. Brucella infection spreads to humans through direct contact with domesticated animals or their products (e.g. unpasteurized milk). Vets, farmers and abattoir workers are at increased risk of infection.
Pathogenesis
Brucellae are able to survive inside the cells of the reticuloendothelial system using superoxide dismutase and nucleotide-like substances to inhibit the intracellular killing mechanisms of their host.
- Intermittent, high fever in the early stages of infection, giving rise to its old name 'undulant fever'.
- Myalgia, arthralgia and lumbosacral tenderness.
- Complications of acute infection that include septic arthritis, osteomyelitis and epididymo-orchitis.
- A chronic infection that may develop without treatment, which may resolve or continue to give symptoms, often accompanied by psychiatric complaints, for many years.
Laboratory Diagnosis
Culture of blood and bone marrow is diagnostic, although culture is less likely to be positive in chronic disease. Incubation, in a high containment facility, must be continued for up to 3 weeks. Serodiagnosis is by enzyme immunoassay (EIA) to detect both IgG and IgM.
Optimal treatment is with tetracycline for 1 month. Streptomycin should be added for patients with complications. Transmission by food can be prevented by pasteurization. Appropriate animal husbandry techniques can reduce the risk of occupational infection. An animal vaccine is available but is not sufficiently safe for human use. Animal control measures have eradicated brucellosis from farms in many countries.
Francisella tularensis
This pathogen of rodents and deer can be found in North America and northern Europe. Infection, which is spread by the aerial route, direct contact with wild animals or by tick bite, is rare, being found mainly in campers and hunters.
Infection may be ocular or localized to the skin, with regional lymphadenopathy. Systemic infection gives a syndrome that resembles typhoid, with 5-10% mortality. Diagnosis is by serology or by culture. Treatment is with tetracycline.
Yersinia
Yersinia pestis
Yersinia pestis infection is described in Zoonoses .
This organism, morphologically and biochemically similar to Y. pestis, causes acute enteritis, mesenteric adenitis and, rarely, septicaemia. It is transmitted to humans in food and water. Infection may be complicated by polyarthritis and erythema nodosum. Patients with iron-overload syndromes are especially susceptible. Diagnosis is by isolation from faeces, blood or lymph node, or detection of antibodies. Treatment with ciprofloxacin or co-trimoxazole is indicated in serious infection; tetracycline is an alternative therapy.
Yersinia pseudotuberculosis
This organism can cause mesenteric adenitis that mimics appendicitis.
Bartonella are small Gram-negative bacteria that can invade host red blood cells, epithelial and bone marrow cells. B. henselae is responsible for cat-scratch disease (see Zoonoses), endocarditis and bacilliary angiomatosis, a febrile illness associated with a red, papular rash that is commonly found in patients with AIDS. B. quintana, which is transmitted by lice, causes a relapsing febrile illness found in severely disadvantaged individuals. B. bacilliformis infection can cause Oroya fever, an acute febrile haemolytic anaemia or mild fever with body pain, nausea and headache. It is transmitted by sandflies and found only in Peru and neighbouring countries. Diagnosis is by culture, but NAATs and sequencing are more sensitive.