Vibrio, Campylobacter and Helicobacter
Vibrio spp.Vibrios are Gram-negative, curved, motile bacilli. There are more than eight species; V. cholerae and V. parahaemolyticus being the main human pathogens.
Vibrio cholerae
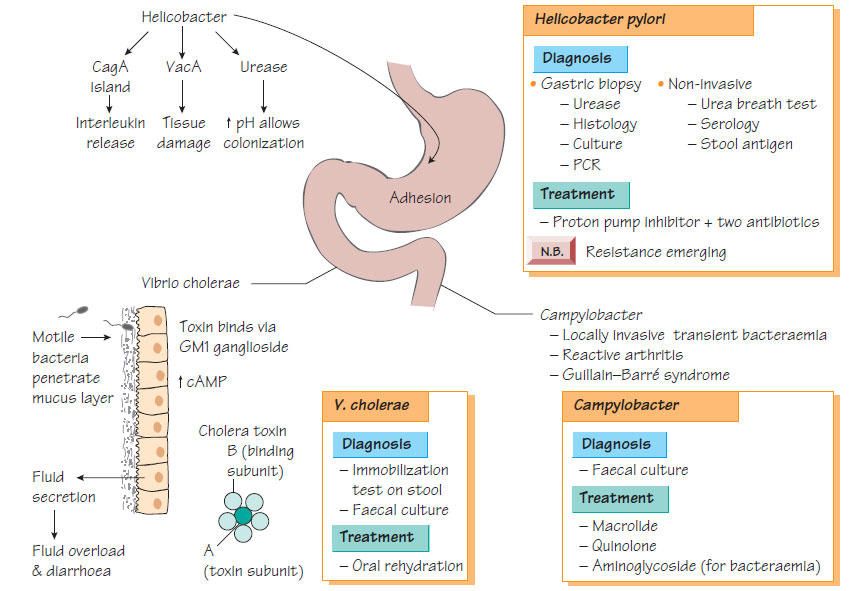
The organism is subdivided by the somatic O antigens; O1 and O139 being the main types associated with cholera. They are able to survive the gastric acidity, burrowing through the intestinal mucus to attach to intestinal epithelial cells via the GM1 ganglioside and produce a multimeric protein toxin (cholera toxin), which stimulates adenyl cyclase within the enteric cells, resulting in the secretion of water and electrolytes into the lumen of the bowel.
- Cholera is an exclusively human illness.
- It is transmitted via contaminated water and food.
- It is usually found in developing countries where there is inadequate sanitation and an unsafe water supply.
- Epidemics are facilitated by war, refugee movements and mass migration.
- Cholera gives rise to periodic pandemics: the most recent epidemic was the seventh recorded.
Clinical features
The clinical features of cholera include:
- massive, painless, fluid diarrhoea (up to 20 L per day);
- vomiting;
- severe dehydration and electrolyte imbalance. However, it can be a mild or asymptomatic condition.
Where cholera is endemic, the diagnosis is based on clinical features. Immobilization of cholera bacteria in a diarrhoeal stool with specific antiserum yields a rapid diagnosis. The organism can be cultivated on specialist medium. Biochemical identification and serotyping should be performed to confirm the diagnosis.
Treatment
- Oral rehydration solution (salt and glucose mix).
- Intravenous fluids for severe cases.
- Tetracycline or ciprofloxacin can shorten the duration and reduce the severity.
Prevention and control
- Safe water supplies are the mainstay of prevention.
- Community education reduces spread.
- Experimental live attenuated and subunit vaccines are under trial.
Campylobacter are associated with diarrhoeal disease and are the commonest cause of intestinal infection. Although there are more than 18 species of Campylobacter, C. jejuni is responsible for 90% of Campylobacter gastrointestinal infections. Infection follows ingestion of contaminated meat, poultry, unpasteurized milk or contaminated water. C. coli causes bacteraemia in immunocompromised patients.
Pathogenicity
Campylobacter jejuni invades and colonizes the mucosa of the small intestine. Antibodies to GM1 ganglioside are associated with Guillain-Barr� syndrome.
Clinical features
- Influenza-like symptoms.
- Crampy abdominal pain.
- Diarrhoea, which may be blood stained.
- Children may be misdiagnosed as appendicitis or intussusception.
- Self-limiting bacteraemia is common.
- Guillain-Barr� syndrome, which is ascending demyelination with motor and sensory deficits following a few weeks after Campylobacter infection, is a rare complication.
- Reactive arthritis may also occur.
- Culture of faeces, or other samples, on specialist medium.
- Identification by morphology and biochemical testing.
Treatment
Diarrhoea is often self-limiting, but patients may be treated with erythromycin or fluoroquinolones. An aminoglycoside may be added for patients who have septicaemia.
Prevention and control
Prevention of campylobacteriosis depends on good animal husbandry and abattoir practices, and on good food hygiene in shops, dairies and the home.
Helicobacter pylori
Helicobacter pylori is a motile Gram-negative, spiral bacillus. H. cinaedi and H. fennelliae have been isolated from patients with HIV infection complicated by proctocolitis and bacteraemia.
Helicobacter pylori expresses urease, which raises the pH in the surrounding locality, therefore protecting the bacterium from the effects of gastric acid. The CagA pathogenicity island encodes a type IV secretion system that injects the CagA protein into the host cytoplasm, where subversion of a variety of cellular functions occurs that results in IL-8 secretion and inflammatory cell recruitment. VacA, a secreted protein that damages cells, is associated with severe disease.
Clinical features
- Often asymptomatic.
- Chronic infection often takes the form of a low-grade gastritis.
- Strongly associated with both gastric and duodenal ulceration.
- Associated with an increased risk of gastric cancer.
Diagnosis
- Culture or nucleic acid amplification test (NAAT) of gastric and duodenal biopsy.
- Urease breath test.
- Stool antigen test.
- Serology, but this cannot distinguish between recent or old infection.
- Proton pump inhibitor, clarithromycin and metronidazole or amoxicillin.
- Specialist advice is required if resistance is suspected.
- Re-infection with H. pylori in adulthood is unusual.