Isolation Techniques for Enteric Pathogens
Bacterial diseases of the intestinal tract can be highly communicable and may spread in epidemic fashion. Their agents enter the body through the mouth in contaminated food or water, or as a result of direct contacts with infected persons. Among the Enterobacteriaceae, the organisms of pathogenic significance belong to the genera Salmonella, Shigella, and Yersinia. Also certain Escherichia coli strains can produce disease by several mechanisms including invading tissue or producing toxins. Such strains are referred to as enteroinvasive or enterotoxigenic, respectively.The many species of Salmonella can be distinguished on the basis of their serological properties as well as their biochemical activities. These organisms characteristically cause acute gastroenteritis when ingested, but some also can find their way into other body tissues and cause systemic disease. Among these, the most important is Salmonella typhi, the agent of typhoid fever, a serious systemic infection. The salmonellae are gram-negative bacilli that are usually motile. They usually do not ferment lactose but display a variety of other fermentative and enzymatic activities.
Shigella species are the agents of bacillary dysentery. These organisms are gram negative and nonmotile. They usually do not ferment lactose. In fermenting other carbohydrates they produce acid but not gas (with one exception). They can also be identified to species by serological methods.
Yersinia enterocolitica is the cause of acute enterocolitis, primarily in children. Its symptoms may mimic those produced by Salmonella, Shigella, or enteroinvasive E. coli. Occasionally, the symptoms are more suggestive of acute appendicitis. The organism grows better at room temperature (25°C) than at 35°C; therefore, it may not be isolated unless the physician notifies the laboratory that yersiniosis is suspected. In this case the isolation plates are incubated at both temperatures. Yersinia are gramnegative bacilli that are motile at 25°C but not at 35°C. They ferment sucrose, but not lactose. Y. enterocolitica is urease positive.
Disease-producing E. coli were once thought to be associated only with epidemic diarrhea in babies, but they are now known to be a common cause of “traveler’s diarrhea” (“turista”) and a variety of other gastrointestinal diseases. Some of these strains may be distinguished from others by immunological typing of cell wall (O) and flagellar (H) antigens. In addition, an enzyme immunoassay is available to detect E. coli toxin directly in stool specimens.
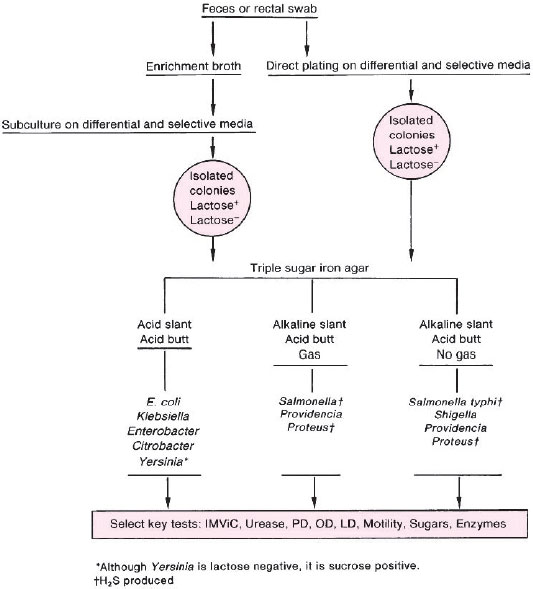 |
| Figure 24.1 Flowchart showing procedures for isolation and initial identification of Enterobacteriaceae by culture. |
The pathogenic Enterobacteriaceae are first isolated from clinical specimens by using highly selective media to suppress the normal flora in feces and to allow the pathogens to grow. Many of these media contain lactose, with a pH indicator, to differentiate the lactose-nonfermenting Salmonella, Shigella, and Yersinia (colorless on these agars) from any lactose-fermenting normal flora that may survive (pink or red colonies see colorplate 16 and 17). EMB or MacConkey agar is commonly used, together with two more highly selective media such as Hektoen enteric (HE) and bismuth sulfite (BiS) agars. In addition, an “enrichment” broth containing suppressants for normal enteric flora may be inoculated. After an incubation period to allow enteric pathogens to multiply, the enrichment broth is subcultured onto selective and differential agar plates to permit isolation of the pathogen from among the suppressed normal flora. Subsequent identification procedures are based on the same types of biochemical tests that you have studied, but may be more extensive to differentiate the enzymatic activities of enteric species that are closely related to Salmonella or Shigella.
Other bacterial pathogens are associated with intestinal disease. Campylobacter jejuni, a curved, gram-negative bacillus, may be the most common bacterial agent of diarrhea in children and young adults (see colorplate 6). It has relatively strict growth requirements and special procedures must be used to isolate it in the laboratory. Some vibrios, notably Vibrio cholerae (the agent of cholera) and Vibrio parahaemolyticus (of the family Vibrionaceae), represent other examples of significant intestinal tract pathogens. These organisms can also be isolated from cultures of fecal material and identified by their characteristic morphological and metabolic properties. Although the choice of isolation media and identification procedures must be varied according to the nature of the organism being sought in a specimen, the principles are the same as those we are following here. You should read further about infectious diseases acquired through the alimentary tract, including bacterial food poisonings, and be prepared to discuss the essential features of their laboratory diagnosis, beginning with the collection of appropriate specimens.
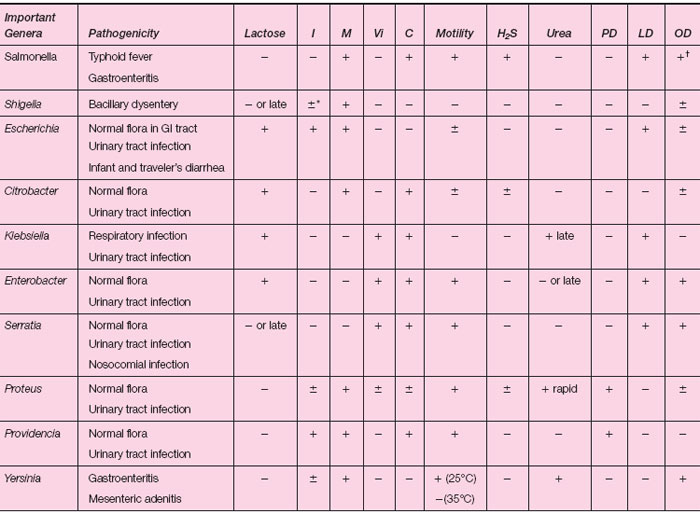 |
| Table 24.2-1 Enterobacteriaceae |
†S. typhi is OD negative
In this experiment and Experiment 24.3 we shall review the basic methods for isolation and identification of enteric pathogens belonging to the genera Salmonella and Shigella. The general procedures are summarized in the flowchart shown in figure 24.1, and the biochemical reactions that you have studied in identifying Enterobacteriaceae are reviewed in table 24.2-1.
| Purpose | To observe the morphology of Salmonella and Shigella species on selective and differential isolation plates |
| Materials | EMB or MacConkey plates Hektoen enteric (HE) plates Bismuth sulfite (BiS) agar plates Agar slant cultures of a Salmonella species and a Shigella species |
Procedures
- Inoculate a Salmonella culture on each of the selective media provided. Streak for isolation. Do the same with a Shigella culture.
- Incubate your six plates at 35°C for 24 hours. Continue the incubation of BiS plates for 48 hours.
- Examine all plates and record your observations under Results.
Results
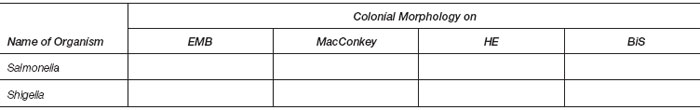 |
Look up the composition of HE agar. List the major ingredients and state why you think they should affect the appearance of Salmonella in the way you have reported.




